The Insurance Stack in a Disrupted World
1 The Insurance Stack in a Disrupted World: the Value, Functional Organization and Role of the Traditional Insurer
DRAFT / work in progress!
Value and Functional Organization in the Insurance Stack With Implications for the Traditional Insurer’s Place in a Disrupted World
Abstract FinTech disruptors are investing billions of dollars attempting to reshape the trillion dollar insurance industry. Do these flows represent and extensional threat to traditional insurers or will they simply lead to incremental improvements? The functions of a traditional property-casualty insurer can be broken into four parts: customer, paper, claims, and capital. These functions are defined, their value quantified, and alternative organizational structure are categorized and classified. Christensen’s theory of disruption is reviewed and applied to the insurance industry. The potential impact of three classes of FinTech investments are analyzed: predictive analytics and granular underwriting, risk analytics and risk shaping, and blockchain and disaggregated trust. Disruptive insurance investments are seen to be largely orthogonal to the functions of a traditional insurer or consistent with them. Where they disrupt core insurer functions directly they face high hurdles from fundamental economic inefficiency, often driven by information asymmetry or morale hazard, or because they undermine the social function of insurance. Traditional insurers serve a unique purpose within a modern economy that is more likely to be helped than hurt by FinTech disruption.”
1.1 Introduction
Globally insurance is a $5 trillion business. Property casualty insurers write $1.4 trillion of premium annually, with over $600 billion in the US. Such a large industry is an obvious target for technology enabled disruptors looking for the “next big thing”. Insurance seems particularly vulnerable having been largely immune to past rounds of dislocation. In the US, insurance was not subject to multiple waves of mergers and acquisitions like the banking industry, for example. The external view of insurance is rarely positive. Insureds complain of onerous and time-consuming underwriting, inadequate coverage concealed in confusing contracts, and unfair claim settlement practices. On its face the industry appears ripe for disruption.
Technology driven disruption picks at individual components of the so-called insurance “stack”, weeding out inefficiencies, duplication, or unnecessary expense. Today’s FinTech startups are challenging all core insurance functions: the Customer function of origination and distribution; the insurance “Paper” function of underwriting and pricing to create and manage a risk pool; the Capital function of risk bearing; and the Claims function of adjusting, settling and paying claims. The first of these, customer origination and distribution, is often outside the tight binding of services provided by a traditional insurer and provides a clear opportunity for FinTech investors.
Relationships between the other three functions, paper, capital and claims, are bound by strong forces to counter the disaggregating pull of technology. These forces control incentive and information problems between the participants: insureds vs. management and management vs. capital providers. Insurer buying motivations, largely the presence of mandatory insurance coverages and the resulting role of insurance within society, create a need for regulation, both of the insured-insurer relationship and of an insurer’s products, behavior and solvency, that in turn place specific constraints on insurer form and operation. As a result, a basic traditional insurer structure has emerged and endured over the last 250 years as a tightly bound amalgam of services operating within a strict incentive control and regulatory framework.
The traditional insurer structure has tight binding between underwriting and pricing, guarding entrance to the risk pool; claims adjusting, guarding exit from the pool; and capital, ensuring a strong foundation. Insureds, participating in a risk pool, must be assured they are treated equitably relative to other pool members, pool management, and outside investor owners. Outside investors, in turn, need to be assured management is aligned with their best interests. As such, underwriting and capital needed generally to be bound under a common management. Claim adjusting, as a discrete, manageable function, can in theory be less tightly bound, but in practice a tight binding is most commonly observed in the marketplace for various good reasons. Within the paper-capital-claims triumvirate there are a range of legal structures, including a mutual insurance company, a reciprocal exchange, a stock insurance company, and a Lloyd’s syndicate, which address insured-manager-owner conflicts in different ways.
Where will technology take the insurance industry? The FinTech universe of startup companies can be categorized and analyzed according to the potential solutions they offer: Internet of things (IOT), telematics, remote-sensing (drones), artificial intelligence, big data, financing, Blockchain, distributed trust, and so forth. An alternative categorization is problem-based. How does startup activity align to industry problems: fundamental problems of information asymmetry, strategic problems, business processes problems and regulation? In addition, how will the industry react to emerging risks thrown off as a corollary of tech-enabled activities such as cyber-risk and sharing economy related exposures. Figure 1 is a schematic of how these problems, solutions and new emerging risks are aligned.
The potential impact of technology on insurance is introduced in Section Section 1.8. Section Section 1.9 then analyzes three particular reference to three applications in detail. The first is the use of predictive analytics enabled granular underwriting to combat the fundamental problems of adverse selection and moral hazard. Secondly, the use risk analytics and risk shaping to address management’s responsibility to assure capital adequacy, and to use capital efficiency. And finally, the use Blockchain and disaggregated trust to help address strategic, operational and regulatory problems.
The analysis concludes that new technology has the potential to revolutionize the underwriting process and that it is sure to enable new insurance products and services, to allow for more customized and granular underwriting, to ease the burden on insurance buyers, to and streamline existing internal processes. It will likely replace and disrupt incumbent many of the industry’s current service providers. But there are meaningful economic reasons why it will not radically alter the fundamental structure of the traditional insurer, a structure that has endured largely unchanged for over 250 years.
The contributions of the paper are…
- enumerating key insurer functions and quantifying the value of each. this expands previous work which looked at aggregate expenses (true?)
- pin pointing the cost of reinsurance and quantifying the proportion of capital provided by reinsurance; work on a direct basis rather than a net basis
- mapping different insurer needs to functional requirements of insurers
- risk shaping analysis of the risk pool and implications for insurability and gain from diversification.
- survey FinTech and InsureTech environments to identify commonalities between startups, map each to the IC value chain and discuss the threat each poses to the traditional stack. Often find the “new” fintech innovation is re-creating an existing insurance structure, for example P2P.
- consider the potential for a jumbo platform to swoop up everything (not likely because of need to understand the deets of each insured)
- meat on bones of blockchain
REGARD CAPITAL as FINTECH and successful for insurers; COST OF CAPITAL = FRICTIONAL COSTS.
The paper is organized as follows. Section 2… Then Sections 3, 4, 5 and 6 follow a common template, providing for each of the Customer, Paper, Capital and Claims
- a detailed description,
- an estimate of its value created,
- a discussing its organizational forms, and
- a summary of market distribution by different forms of organization.
- problems faced by insurers
- solutions offered by FinTech
- detailed analysis of pred modeling, risk shaping, and block chain
- conclusion.
1.2 Value and Organization of the Insurance Stack
1.2.1 Overview
The Property-casualty insurance value-chain, or “stack” in FinTech-speak, consists of four primary functions.
- The Customer function of origination and distribution: including insured acquisition, marketing, sales, education, needs analysis, servicing.
- The Paper function of underwriting and pricing to create and manage a risk pool: including the creation of an insurance entity serving as the paper that is the counter-party to insurance contracts that meets insured needs for risk transfer and for statutorily and contractually required insurance; and for the creation and management of a fair, efficient and solvent risk pool.
- The Capital function of risk bearing: that ensures adequate, liquid financial resources are available to guarantee claims paying ability for the risk pool.
- The Claims function of adjusting, settling and paying claims.
An investment or intermediation function is often considered core, but for property-casualty insurers, which deal with short duration contracts, it is of second-order importance as a function. It is, however, a material source of revenue. The analysis below will make the simplifying assumption that insureds are credited with investment income on funds they provide at the average rate the insurer earns on its invested assets. The investment function creates value if it earns a higher rate on assets than is credited to insureds.
Having identified the components of the insurance stack, the next challenge is to quantify each component’s output value. Insurance companies produce services, many of which are intangible and hard to value. In the literature there are three principle approaches used to measure financial service firms output value (Cummins and Weiss 2013).
The first is the intermediation approach, which applies to pure financial intermediaries and considers the spread earned on assets over the cost of funds used. Since property-casualty companies are only incidentally intermediaries and since they also provide other real risk management services the intermediation approach is not appropriate.
The second is the user-cost method, which considers the financial returns on each product. This method requires precise revenue and cost information by product that is generally not available for insurance products, which are often complex bundles of different services.
The third approach is the value-added approach, which (Cummins and Weiss 2013) explain is the most appropriate method for property casualty insurers. The value-added approach judges the value added by an expense category using operating cost allocations. Why does this approach make sense? According to (Kenneth Joseph Arrow et al. 1974) the value of risk pooling to insureds is the maximum they will pay in addition to the expected loss amount transferred to the pool. At any higher premium the insured can refuse to buy insurance, although this may not be an option for mandatory insurance. In a competitive market the actual premium charged will generally be lower than the maximum because insurers are risk neutral relative to small, independent claims. Therefore the excess of premium over expected losses represents value added by the insurer through pooling. Prospectively this excess is exactly non-loss expenses plus the expected cost of risk-bearing capacity in the pool.
(Cummins and Weiss 2013) regard insurers as providing three principle services.
- Risk-pooling and risk-bearing. The cost of operating the risk pool include actuarial, underwriting, product development, and regulatory and rating agency compliance activities.
- “Real” financial services relating to insured losses. These services include risk surveys, needs analysis and coverage design, and loss prevention services.
- Intermediation. Intermediation services are incidental to property-casualty business. Policyholders receive a discount in the premium to compensate for the opportunity cost of the funds held by the insurer. Any margin between the rate of return earned on assets and the rate credited to policyholders in premium represents a value-add of the intermediation function.
The first function is equivalent to the Paper function. The second combines aspects of of Customer and Claims. (Cummins and Weiss 2013) report that in 2010 property-casualty companies incurred $178.7 billion of expenses. Commissions and brokerage accounted for 25.1 percent and claim adjustment services for 13.5 percent of the total. Taxes licenses and fees were 6.3 percent. However, their remaining expense items are broken out by expense category, such as employee salaries and benefits or advertising, rather than insurer value-add function. They also reported a cost of capital of 13 percent, applied to equity capital of $580.5 billion, giving and equity cost of capital of $75.5 billion.
The next sub-section describes how this theory will be applied to each function, using publicly available information to estimate its value.
1.2.2 Quantifying Value by Function: Methodology
This section explains how publicly available information is used to estimate the value of each component of the insurance stack. Customer, Paper and Claims expenses are estimated directly from US statutory financial filings. They are reported by line by calendar year. The reinsurance expense sub-component of Capital can be estimated by line by year subject to a small caveat. Equity capital can only be estimated canonically in the aggregate. Therefore the following presentation shows more detail for the Customer, Paper, Claims and reinsurance-capital components than for total Capital. Section Section 1.5.3 explains the approach for equity capital.
The relevant statutory filing is the NAIC Insurance Expense Exhibit (IEE). The IEE explicitly quantifies Customer, Paper and Claim function expenses by line of business by calendar year. The IEE is produced on a direct and net (that is, direct plus assumed reinsurance minus ceded reinsurance) basis and so it is also possible to quantify the net cost of reinsurance as the difference between direct underwriting results and net underwriting results.
The IEE breaks expenses into the following functional categories, which are mapped to source of value created by insurance services as follows.
- Losses: losses are a transfer and not a part of the value created by insurers (Cummins and Weiss 2013).
- Loss adjustment expenses, which are subdivided into defense and cost containment, covering specific claim-level costs such as attorney fees, and adjusting and other expenses. Loss adjustment expenses create the value of the Claim function.
- Dividends to policyholders: dividends are part of product design and marketing. They are part of the Customer function.
- Commission and brokerage expense is also part of the Customer function.
- Taxes licenses and fees are regarded as part of the Paper function, since they largely accrue from regulation. Choice of domicile and regulator is a strategic decision for an insurer, and some select to domicile in low tax jurisdictions to avoid these costs.
- Other acquisition, field supervision and collection expenses, covering the cost of managing the distribution plant. These are part of the Customer function.
- General expenses incurred in underwriting, pricing, product management, accounting, reporting and compliance. These are core to the Paper function.
- Other income less other expenses. The principle source of other income is installment fees on premium payments. The principle other expense is premium written off. These relatively minimal in the aggregate and are included in the Customer function. XXXX
Investment related expenses are netted out of investment income, which in turn is used as an offset to the cost of capital on investor provided funds. Since investment intermediation is not regarded as a core function, investment costs are not explicitly quantified. (Aon Benfield 2016) estimates they are 1.3% percent of total premium and 0.7% of net earned premium.
By providing a consistent functional breakdown, consistent with the core services bundled by insurers, the tables in this section improve on (Cummins and Weiss 2013) Table 1. That table mixes reporting expense functions, such as commission and brokerage and claims adjustment, with expense types, such as employee salary and benefits, advertising and taxes.
The reporting of net reinsurance cost in Section Section 1.5.4 is new. It confirms general market perceptions and is consistent with practitioner sentiment by line. Surprisingly, Statutory and GAAP accounts do not provide a clear statement of the net cost or benefit of reinsurance. However, overall ceded result by calendar year are computed by combining the direct and net IEEs. It is not possible to create ceded results by accident year directly but results for some lines can be estimated on an accident year basis by combining the IEE with Schedule P. The IEE-based reinsurance expense analysis is described in more detail in Section Section 1.5.4.
1.2.3 Functional Organization: Overview
The range of organizational structures within the insurance industry is perhaps the broadest of any major industry. Included are Lloyds associations, where insurance contracts are offered by individual underwriters, stock companies that employ the standard corporate form, mutuals and reciprocals that are more like cooperatives where customer and ownership functions are merged. (Mayers and Smith 1988)
Insurance is a complex business that bundles different functions and services, bought for different reasons, and marketed in different ways. The bundling and marketing are generally intermingled and are often implicit, obscuring underlying functionality and making it difficult to understand and categorize the different structures.
In order to clarify and enumerate the maze of marketed insurance products and services it is first necessary to separate sales and marketing, i.e. the Customer function, from the remaining three functions. Sales and marketing are the face of insurance to the public. Insureds are apt to confuse their broker or agent for their actual insurance company, a confusion perpetuated by brokers and agents who “own the renewal” and strive to control communication with their clients. Organizational forms are described by function below, for Customer in Section Section 1.3.3, Paper in Section Section 1.4.3, Capital in Section Section 1.5.5, and Claims in Section Section 1.6.3.
1.2.4 Market Distribution by Type of Insured
Table 1 reveals Personal lines account for 56% of net earned premium and commercial lines 37%, with the remainder reinsurance. However, personal lines predominating companies account for only 43% of surplus compared to 42% for commercial lines and 22% reinsurers reflecting the lower leverage ratio for commercial lines, and substantially lower than leverage ratio for the insurance companies. Commercial lines companies account for 48% of total assets 59% of loss reserves compared to 58% and 30% respectively the personal lines companies, reflecting the longer payout patents of commercial lines.
Table 2 shows combined Customer, Paper, and Claim expenses are highest for commercial lines companies, as 39.1% of net earned premium, compared to 35.4% for personal lines and 34.9% from reinsurance companies. Customer costs are roughly equal for personal and commercial lines companies, which is a surprising balance of many offsetting factors. Paper costs are three percentage points higher for commercial lines companies reflecting lower volumes across a more complex array of filed and regulated products producing higher average costs. Claim expenses are broadly comparable.
Reinsurance companies have a higher Customer expense reflecting ceding commissions paid to primary companies to reimburse their production costs. Reinsurers have much lower Paper costs reflecting the lack of regulation in the reinsurance industry as well as higher average policy premiums. Claim expense is also lower, reflecting higher average claim size.
| Type of Insured | Net EP | Percent Total | Surplus | Percent Total | Total Assets | Percent Total | Loss Reserves | Percent Total | Lever-age |
|---|---|---|---|---|---|---|---|---|---|
| Personal | 298.1 | 56% | 313.7 | 43% | 731.5 | 38% | 193.3 | 30% | 0.95 |
| Commercial | 196.0 | 37% | 307.5 | 42% | 921.5 | 48% | 372.7 | 59% | 0.64 |
| Reinsurance | 39.5 | 7% | 163.5 | 22% | 316.7 | 16% | 70.2 | 11% | 0.24 |
| Industry | 533.5 | 100% | 735.0 | 100% | 1,920.1 | 100% | 636.2 | 100% | 0.73 |
| Type of Insured | Customer | Paper | Claims | Sum |
|---|---|---|---|---|
| Personal Lines | 17.8% | 6.2% | 11.4% | 35.4% |
| Commercial Lines | 17.5% | 9.3% | 12.3% | 39.1% |
| Reinsurance | 23.7% | 2.6% | 8.6% | 34.9% |
| Industry | 18.1% | 7.0% | 11.5% | 36.7% |
| Risk Retention Grp | 6.6% | 12.9% | 24.9% | 44.4% |
SM IRS 2016 thought somewhere? This is a perverse metric of value…
The overall expense load is very high, standing at 56 percent of earned premium. Put another way, the industry is only paying out 44 cents in loss payments for each dollar of premium. By comparison, the Affordable Care Act requires insurers spend at least 80 percent or 85 percent of premium dollars on medical care. If an insurer fails to meet its applicable minimum loss ratio for a given year it will be required to provide a rebate to its customers.
The Customer link consumes over one third of total expense dollars. Given that up to 60 percent of total premium is mandated, either by law or contractually, and so not the traditional “sold not bought” insurance model, it will be no surprise that a majority of disruptive start-ups target customer acquisition and distribution, particularly in the lower-need, personal lines and small commercial lines segments of the market.
1.3 Value and Organization of the Customer Function
1.3.1 Description of the Customer Function
The Customer function of origination and distribution provides real financial services related to insured risk management, sales and marketing includes the following.
- Customer discovery and education.
- Advertising, marketing and sales.
- Aggregation and quoting engines.
- Risk surveys, risk appetite and needs analysis.
- Risk control and engineering studies.
- Loss prevention surveys and related services, such as workplace ergonomics and health and safety studies.
- Insurance coverage design, including appropriate contract wording, deductibles and policy limits.
- Information management, including gathering and organizing underwriting information.
- Some post-binding customer servicing, including endorsement processing and billing, is often included in the customer category.
For US property-casualty insurers Customer costs account for nearly PP percent of total expenses.
Customer function activities are performed by a variety of entities including independent agents and brokers, tied agents, managing general agents and managing general underwriters, wholesale brokers, risk consultants, and insurer Internet and direct response service representatives. Insurers pay for the services through commission and brokerage and other acquisition, field supervision and collection expenses.
Customer function expenses are computed from the IEE by combining
- Commission and brokerage expenses plus
- Acquisitions, field supervision and collection expenses plus
- Dividends to policyholders plus
- Other expenses net of other income. XXXX
Customer function expenses can be computed by line of business.
Obviously deducting other income minus other expenses is equivalent to adding other expenses net of other income.
Customer function expenses are dominated by external commission and brokerage costs, accounting for nearly 60 percent of the total. People costs account for over 20 percent.
1.3.2 Value of the Customer Function
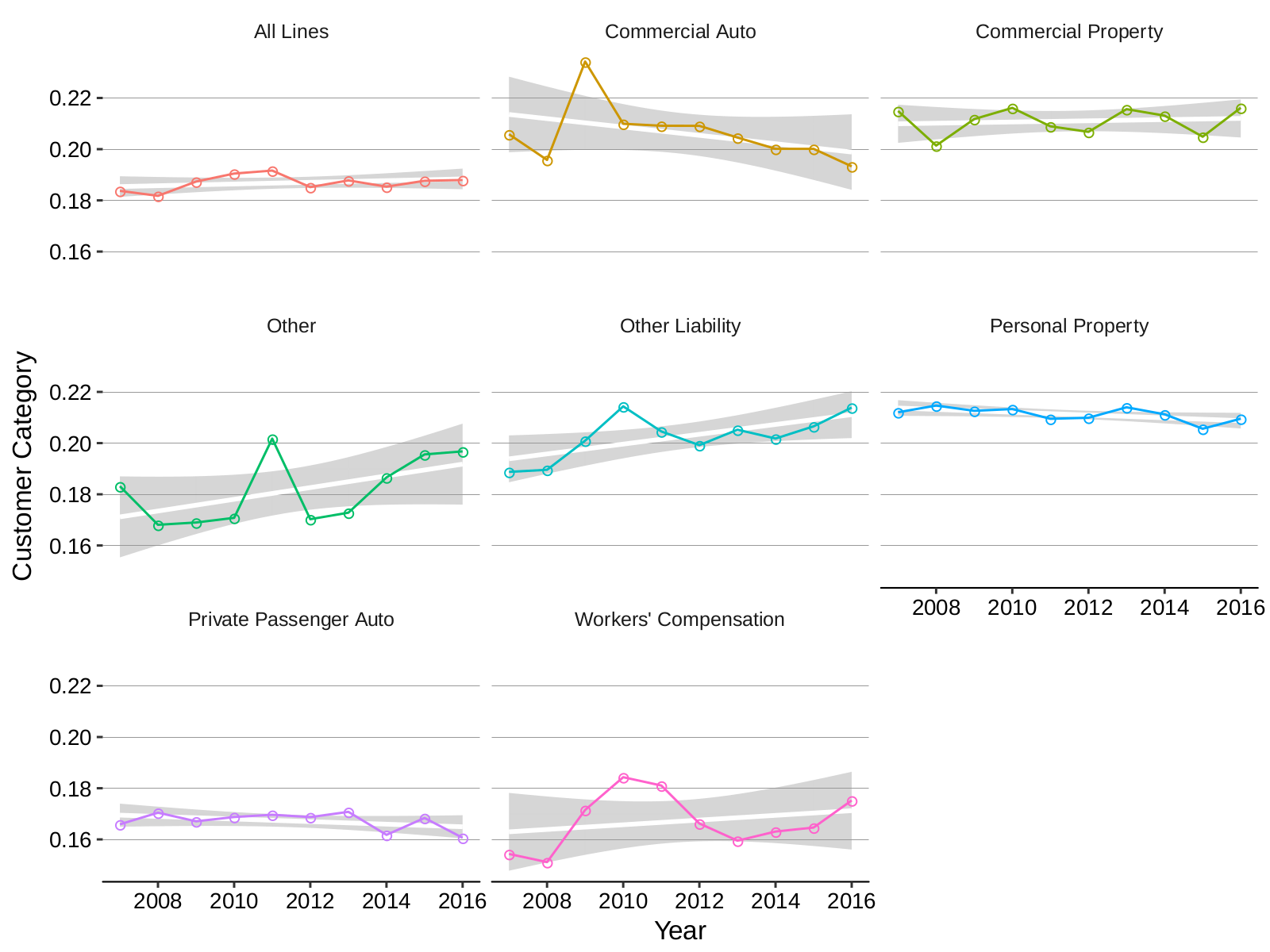
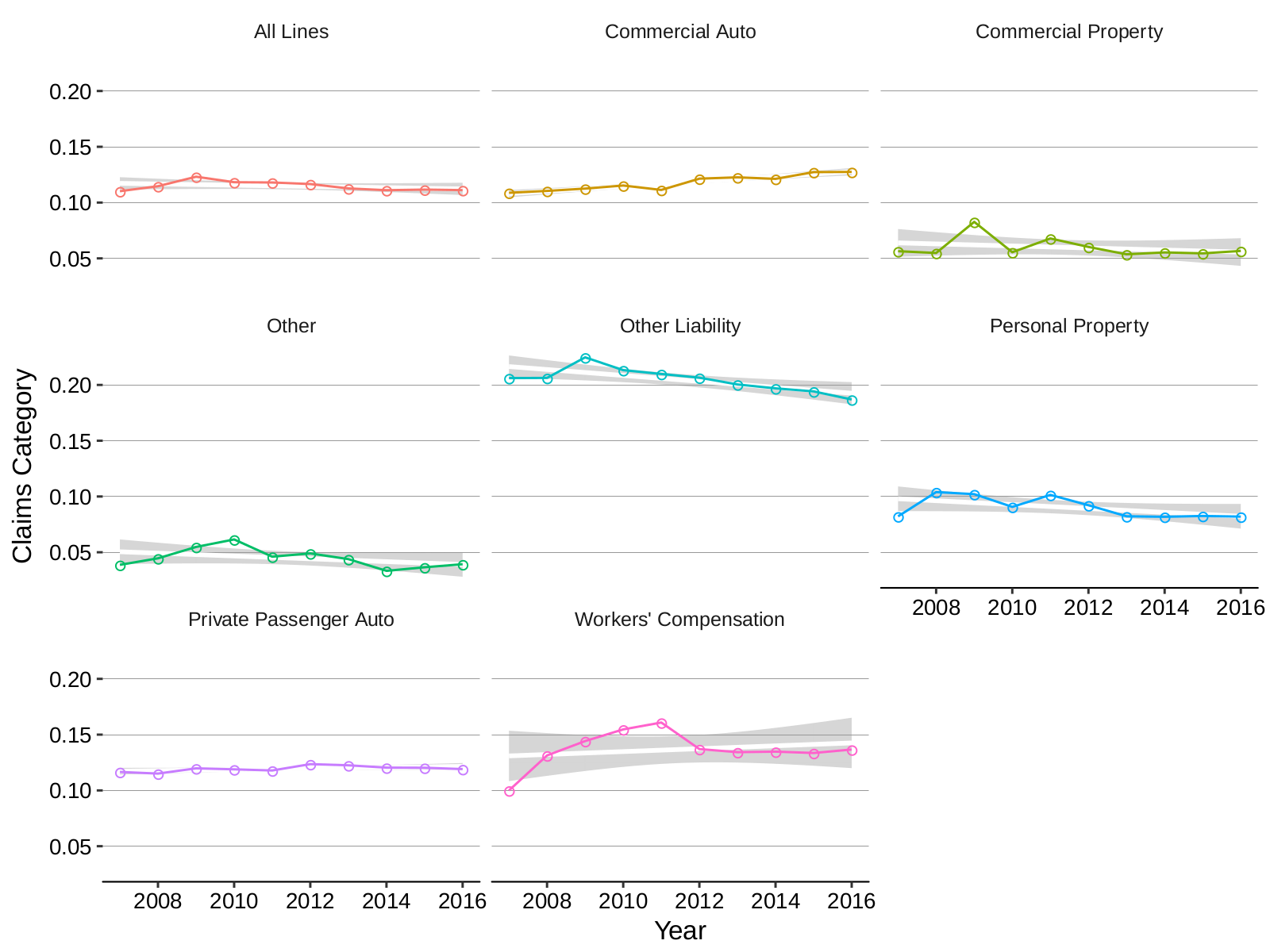
Customer function expenses as a percentage of direct and premiums are shown in Table 3 and Table 3. Across all lines customer related expenses vary less than 0.5 percentage point, from a low of 18.6% in 2009 to a high of 19.1% in 2013. There has been greater variation within the individual lines. Expenses in Personal property, predominantly homeowners, have declined one percentage point, but over this period ates have increased substantially driven by straight-line wind and tornado hail losses. Commercial property expenses have increased by 0.8 percentage points, even though they have been subject to the same rate trends. Private passenger auto, the largest single line, has shown a decreasing trend especially since 2013. Workers compensation has the lowest customer expenses of any category, reflecting the regulated nature of the line and the high average premium per policy.
| LINE | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|---|---|---|---|
| All Lines | 0.184 | 0.182 | 0.187 | 0.190 | 0.192 | 0.185 | 0.188 | 0.185 | 0.188 | 0.188 |
| Commercial Auto | 0.206 | 0.196 | 0.234 | 0.210 | 0.209 | 0.209 | 0.205 | 0.200 | 0.200 | 0.193 |
| Commercial Property | 0.215 | 0.201 | 0.212 | 0.216 | 0.209 | 0.207 | 0.216 | 0.213 | 0.205 | 0.216 |
| Other | 0.183 | 0.168 | 0.169 | 0.171 | 0.202 | 0.170 | 0.173 | 0.187 | 0.196 | 0.197 |
| Other Liability | 0.189 | 0.190 | 0.201 | 0.214 | 0.205 | 0.199 | 0.205 | 0.202 | 0.207 | 0.214 |
| Personal Property | 0.212 | 0.215 | 0.213 | 0.213 | 0.209 | 0.210 | 0.214 | 0.211 | 0.206 | 0.210 |
| Private Passenger Auto | 0.166 | 0.170 | 0.167 | 0.169 | 0.170 | 0.169 | 0.171 | 0.162 | 0.168 | 0.161 |
| Workers’ Compensation | 0.154 | 0.151 | 0.172 | 0.184 | 0.181 | 0.166 | 0.160 | 0.163 | 0.165 | 0.175 |
1.3.3 Organization of the Customer Function
Insurance is inherently specialized. Unlike other products, where the seller does not care about buyer characteristics other than their ability to pay, an insurer must understand its buyer’s characteristics. This need-to-know results in a bewildering array of marketing mechanisms each targeting a different type of insured.
Insureds are identified and segmented using social, demographic and geographic variables. They are often targeted through their employer, affinity organizations, or other associations, an approach generically referred to as “program business”.
Separately, insureds select a distribution channel:
- an independent agent, who represents many insurance companies,
- a tied agent, who represents one insurance company sometimes as an employee,
- a broker, who represents the insured directly and who generally transacts business with several insurance companies,
- an Internet marketing mode,
- direct channels such as telephone or direct mail, or
- a combination of these channels.
In addition there is retail and wholesale distribution. Main Street, vanilla, or standard risks typically approach the insurance market through the retail distribution channel. Specialty, complex, or nonstandard risks often work with a retail producer who then uses a residual market mechanism or the wholesale sub-channel in order to meet insured needs. Thus an agent can be a retail or wholesale agent, the former dealing directly with insureds and the latter with retail agents on behalf of their insureds.
These arrangements are summarized in Figure 3
The requirement that an insurer understand its insureds’ operations is expensive and resource intensive. Larger, risk-homogeneous classes offer the potential for lower average cost of acquisition and underwriting. As a result, it becomes cost effective to invest more heavily in automated distribution and underwriting systems. Internet and direct response models have high fixed cost and low variable costs. They require significant upfront investment and are therefore only cost-effective for large classes of insureds: predominantly personal auto, but moving to include homeowners and small commercial lines insureds. At the other end of the spectrum, small risk-heterogeneous classes are served by low fixed cost, variable cost driven agencies. However, it is possible to abstract many of the steps involved in the acquisition and underwriting of a small class into a process, which can then be customized easily to the particulars of the class. This is the operating model of program managers and managing general agents. It leverages a common platform to market dozens of different affinity or association-based programs. For example AmWins Group Inc., offers 31 different programs on its website including demolition contractors, equine liability, roofing operations, waste haulers, and woodworking operations. These examples show that insurance-related information technology investment ranges from a deep but narrow investment to serve a large homogeneous class to a broad but shallow investment in a platform capable of serving many different heterogeneous classes with minimum customization.
1.3.4 Market Distribution by Customer Function Organization
Table 4 shows the market supports direct distribution and independent channels in approximately equally: agency distribution accounts for 45% of total net earned premium, direct 52% and 3% other. Agency companies have higher than average leverage. They also have a proportionately much higher percentage of total loss reserves, reflecting their historical skew towards larger commercial lines accounts. Broadly, insureds with more complex risk assessment, management and transfer needs skew towards the independent channel.
Table 5 shows direct marketing companies enjoy a full percentage point expensive advantage over agency companies, two percentage points from lower Paper costs, 1.7 percentage points from lower Customer costs, and the remainder from lower Claims costs. The lower Paper costs gain reflects direct marketing’s skew to higher-volume personal lines.
| Marketing Type | Net EP | Percent Total | Surplus | Percent Total | Total Assets | Percent Total | Loss Reserves | Percent Total | Lever-age |
|---|---|---|---|---|---|---|---|---|---|
| Agency | 242.0 | 45% | 290.4 | 40% | 906.3 | 47% | 373.0 | 59% | 0.83 |
| Direct | 275.3 | 52% | 417.1 | 57% | 944.4 | 49% | 243.6 | 38% | 0.66 |
| Other | 16.2 | 3% | 27.5 | 4% | 69.4 | 4% | 19.6 | 3% | 0.59 |
| Industry | 533.5 | 100% | 735.0 | 100% | 1,920.1 | 100% | 636.2 | 100% | 0.73 |
| Marketing Type | Customer | Paper | Claims | Sum |
|---|---|---|---|---|
| Agency | 19.1% | 8.0% | 11.6% | 38.7% |
| Direct | 17.4% | 6.0% | 11.4% | 34.7% |
| Other | 17.2% | 11.5% | 12.2% | 40.9% |
| Industry | 18.1% | 7.0% | 11.5% | 36.7% |
1.4 Value and Organization of the Paper Function
1.4.1 Description of the Paper Function
The Paper function of underwriting and pricing to create and manage a risk pool includes costs associated with the design, delivery and maintenance of insurance products meeting insured risk transfer and required insurance needs. Its duties include the following.
- Product design, including actuarial, statistical, legal, and underwriting policy.
- Product filing, including rate and rule filings and underwriting guideline filings.
- Pool marketing strategy, especially important for direct companies.
- Evaluating risk-pool capital requirements to meet regulator, rating agency and insured economic needs.
- Designing, implementing and maintaining the most efficient risk-pool capital structure using different instruments. The actual costs of the risk capital, that is the actual risk margins, are included in the Capital function. But, for example, costs of a ceded reinsurance department to manage the purchase of catastrophe reinsurance is included in Paper.
- Rating agency relations, meetings and compliance efforts that are part of maintaining the desired risk-bearing rating.
- Investor and reinsurer relations that are part of maintaining the desired risk-bearing capital pool.
- State regulatory compliance audits and market conduct exams, for example the triennial audit.
- Accounting and statutory financial filings
- Enterprise risk management and Own Risk Solvency Assessment (ORSA) processes and documentation, which have recently become more onerous for insurers.
- Management, internal audit and policy oversight of the Paper category organization.
- Taxation of insurance premiums, which is often a byproduct of regulation, and other related licenses and fees are included in Paper.
- Line underwriting and actuarial functions to ensure fair and diligent underwriting, pricing and administration of individual risks in the pool/
- Customer servicing, processing policy coverage changes and endorsements, other than Claims, which are handled separately.
- Customer billing and premium collection.
- Policy and documentation issuance, such as SR-22 cards for auto insurance.
The last four functions are sometimes shared with the Customer category.
For US property-casualty insurers Paper costs account for nearly 25 percent of total expenses.
Paper function activities are generally performed by an insurer. They can be shared with agents and brokers, reinsurers, and captives.
Paper category expenses are computed from the IEE by combining
- Taxes licenses and fees plus
- General expenses minus
- Other income was other expenses. TAKEOUT
Paper category expenses can be computed by line of business.
These functions are very people-intensive and direct people costs, including salary, benefits and payroll taxes, account for 60 percent of Paper category expenses. IT related costs account for 10 percent.
1.4.2 Value of the Paper Function
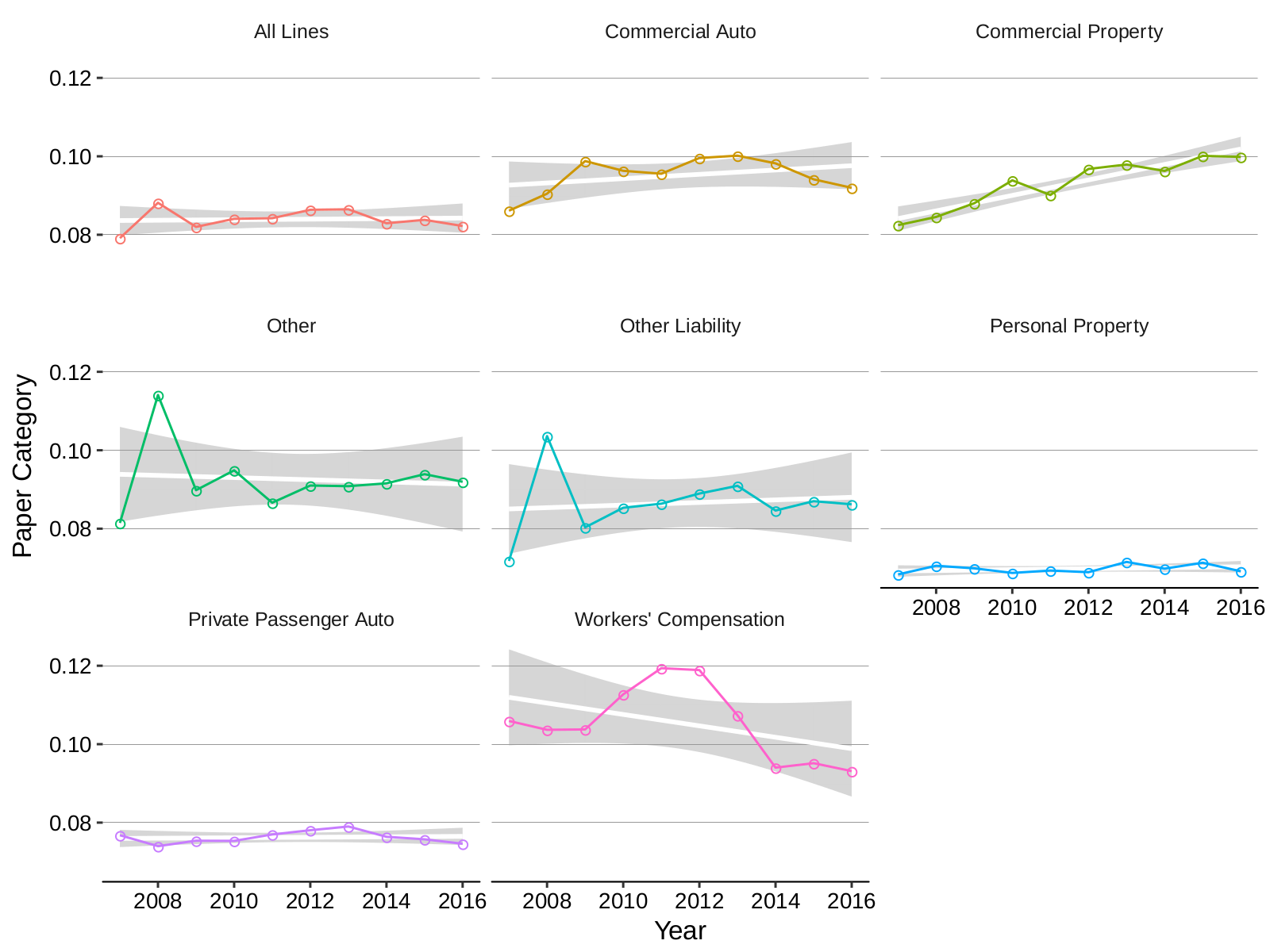
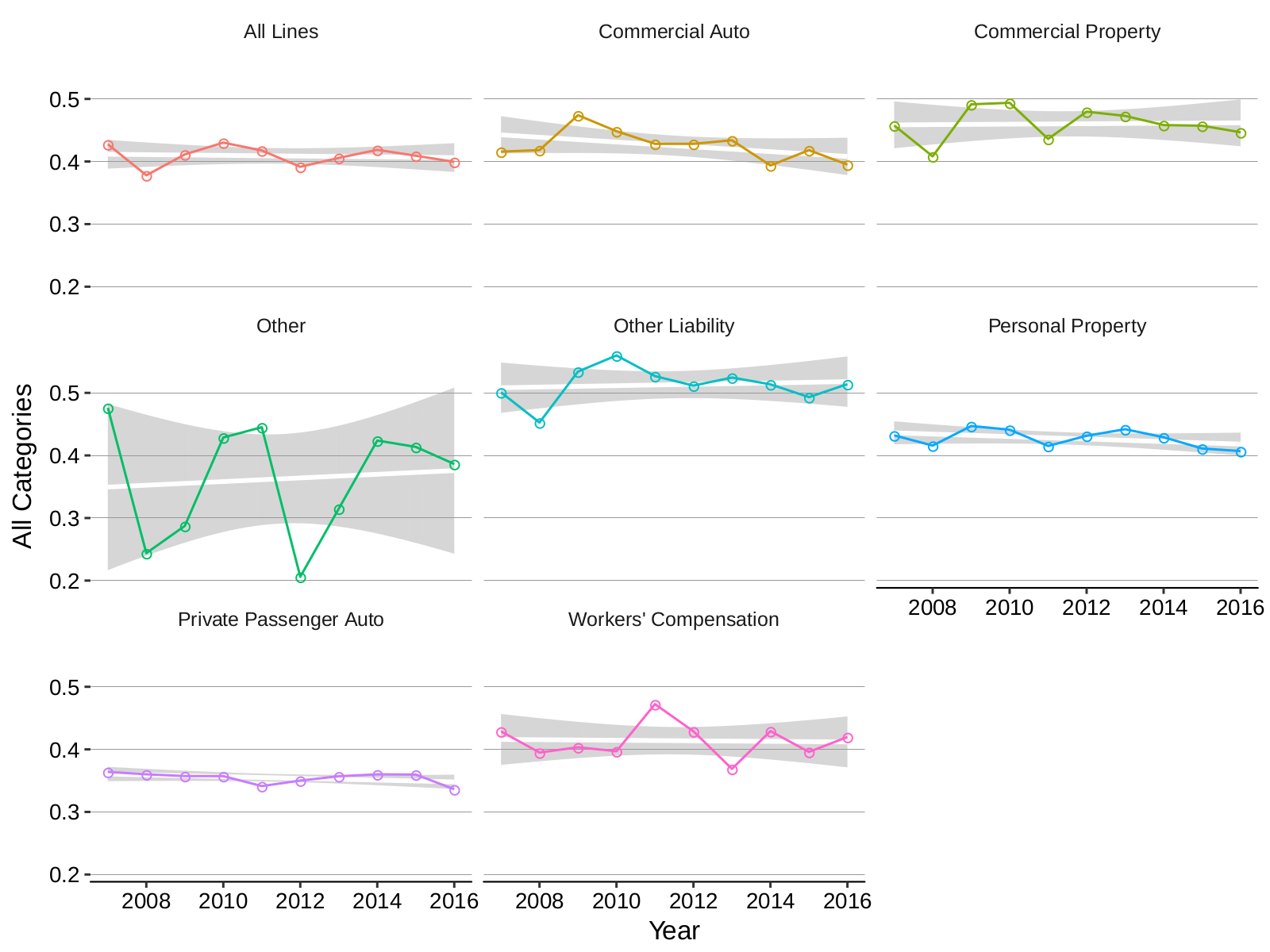
Paper category expenses as a percentage of direct and premiums are shown in Table 6 and Table 6. Paper category expenses have been similarly stable, with all lines expense of 8.4% in 2009 and 2016. Personal lines, personal property and private passenger auto, have lower than average paper costs of around 6.9%, reflecting the large-scale, which produces a lower average filing and regulatory costs, and the prevalence of automated, low-touch machine-driven underwriting. Higher paper costs associated with commercial lines are driven by the complexity of maintaining many different filed rates, some of which will only apply to small lines, and the manual underwriting process, especially for individually risk rated large accounts.
| LINE | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|---|---|---|---|
| All Lines | 0.079 | 0.088 | 0.082 | 0.084 | 0.084 | 0.086 | 0.086 | 0.083 | 0.084 | 0.082 |
| Commercial Auto | 0.086 | 0.090 | 0.099 | 0.096 | 0.096 | 0.100 | 0.100 | 0.098 | 0.094 | 0.092 |
| Commercial Property | 0.082 | 0.085 | 0.088 | 0.094 | 0.090 | 0.097 | 0.098 | 0.096 | 0.100 | 0.100 |
| Other | 0.081 | 0.114 | 0.090 | 0.095 | 0.087 | 0.091 | 0.091 | 0.092 | 0.094 | 0.092 |
| Other Liability | 0.072 | 0.104 | 0.080 | 0.085 | 0.086 | 0.089 | 0.091 | 0.085 | 0.087 | 0.086 |
| Personal Property | 0.068 | 0.071 | 0.070 | 0.069 | 0.069 | 0.069 | 0.072 | 0.070 | 0.071 | 0.069 |
| Private Passenger Auto | 0.077 | 0.074 | 0.075 | 0.075 | 0.077 | 0.078 | 0.079 | 0.076 | 0.076 | 0.075 |
| Workers’ Compensation | 0.106 | 0.104 | 0.104 | 0.113 | 0.119 | 0.119 | 0.107 | 0.094 | 0.095 | 0.093 |
1.4.3 Organization of the Paper Function
Somewhere: hence ins is a relationship business!
The organization of the Paper function is by far the most complex of the four. As a result this Section is the heart of the first half of the paper.
Risk pooling creates value for risk averse pool members. However, there is a cost associated with the creation and management of a risk sharing pool. Each member of potential member of the pool must be assured that all members are being treated equitably, particularly if individual members have heterogeneous risk profiles. The pool manager must credibly assess and charge for individual member risk, through underwriting. The pool manager must ensure claims are adjusted fairly both from the perspective of the policyholder, the claimant, and all other pool members. Finally, the pool manager must ensure the pool has adequate risk bearing financial resources to meet its member claim obligations. In theory underwriting and pricing, claim adjusting, and risk bearing could be disaggregated and handled by separate organizations. However, disaggregation brings morale hazard between all three of these interrelated risk pooling functions.
Disaggregated pricing and underwriting are observed in the managing general agency and managing general underwriting models. MGAs and MGUs are most common in specialty markets paying a premium to distribution. The contractual arrangements between the MGA/U and the risk bearing entity are closely negotiated and carefully monitored, both sides being aware of potential abuses. SORT OUT ORDER
Many insurance products are required by law or by contract, often for the protection of third parties. As a result there are regulations in place to ensure insurance contracts effectively provide the expected protection.
There are many examples of required insurance.
- Liability insurance is required to operate a motor vehicle.
- Workers compensation insurance is required to protect workers injured on the job.
- General liability insurance is often required of contractors to protect the principal.
- Surety insurance is required in many contracts.
- Collateralized debt contracts usually require insurance protection of the underlying collateral, for example mortgagors require lenders maintain homeowners insurance and auto loans require collision and comprehensive physical damage cover.
Approximately 65 percent of property-casualty premium is accounted for by lines of business that it is mandatory for insureds to purchase, 32 percent by lines with some mandatory component, and only 3 percent fully voluntary, see table XX.
Since a mandated insurance separates the ultimate beneficiary of the insurance from the purchasing decision-maker it creates a need for independent, objective regulation to ensure the existence of insurance meeting the legal and contractual requirements. Regulation is also beneficial for first party coverages when the decision-maker lacks the expertise to evaluate insurer solvency.
Regulations governing allowable underwriting and pricing variables, sales practices, claims handling practices, and contract terms and conditions for mandated covers are commonly observed in major markets.
Insurer financial solvency regulation is also global phenomenon and all developed insurance markets have statutorily defined minimum capital requirements. These conditions can be supplemented with oversight by quasi-official rating agency organizations, which place a very real extra burden of compliance on insurance companies.
Insured needs, and resulting demand, interacts with Capital supply considerations within the Paper function to determine the form and organization of an insurer, see Figure 5. These two sets of constraints and their interaction considered in the next three subsections.
Insured Demand: Meeting Insured Needs
An insured can purchase insurance to meet one or more of the following needs needs.
- Satisfying: (Kunreuther et al. 2013) the insurance policy satisfies certain statutory, regulatory, or contractual requirements in order for the insured to carry out another activity. Financial responsibility laws for driving an automobile and employer liability laws are examples of statutory requirements. Debt contracts requiring insurance protection of are an example of a contractual requirement. If insurance must meet a satisfying requirement then the insurance policy must be issued by an entity complying with the appropriate laws, regulations, and rating agency restrictions.
- Risk pooling: is the classic motivation for risk averse individuals to purchase insurance. The insured is exposed to a material risk which they wish avoid. Diversification allows them to do this by pooling their risk with other insureds. Risk pooling is the magic ingredient of insurance. An efficiently run risk pool replaces each insured’s uncertain loss outcome with a more certain pool average value, plus an expense load. It is well-known in insurance economics this pooling creates substantial value for risk averse insureds CITATION NEEDED. Risk pooling is clearly inter-insured. Property-casualty insurance, typically written with a short duration one year or less contract, is therefore essentially intra-temporal. Life insurance, often written with very long duration contracts, is inter-temporal. Life products can be either inter-insured (traditional term and whole life, and annuities) or intra-insured (variable annuities).
- Risk financing: the insured seeks to finance uncertain future contingencies in an efficient manner. Risk financing requirements are typically driven by accounting regulation and tax law. Under GAAP an obligation cannot be expensed unless it is reasonably certain in timing and amount. A future payment to settle a lawsuit may not meet these requirements and so may not be a deductible expense. Insurance premium, subject to certain restrictions, is a deductible expense, both for reporting income and for tax purposes. Insureds seek risk financing structures allowing uncertain future expenses to be fully deductible. Risk financing is typically performed for a single entity over time, it is inter-temporal, intra-insured. The risk financing requirement is generally to fund the known or certain part of losses in a cost efficient manner. Large deductibles, self-insured retentions and captives are used to satisfy the risk financing need.
There is no bright line distinction between risk financing and risk pooling. Risk financing issues become evident for larger insureds, often signaled by discussion of “dollar swapping.” Dollar swapping refers to premiums paid to the insurer that are almost certain to be returned as loss payments, less taxes, commission and expenses: clearly inefficient from the insured’s perspective. Larger insureds attempt to minimize overall “total cost of risk” by avoiding these administrative markups on predictable loss payments, restricting their insurance purchase risk pooling for to less frequent, higher severity loss events. FORWARD REF TO MORE TREATMENT?
Risk liquidity, the need to have liquid assets available to pay a loss when due, is another potential need met by insurance. For example, an insurance company with a large stock portfolio has a motivation to purchase catastrophe reinsurance so it cannot be forced to liquidate stocks to pay for unexpected catastrophe losses in a bear market. The liquidity need is generally met either as a corollary of risk pooling or is subsidiary to risk financing and so it will not be treated separately.
Table 7 provides examples showing each of the three primary needs satisfying (Sat), risk pooling (RP) and risk finance (RF), are independent and that all seven possible combinations of needs exist and are met in the market.
| Insured group or insurance product | Sat | RP | RF |
|---|---|---|---|
| Non-standard auto | x | ||
| General liability for judgment proof corporation | x | ||
| Term life insurance | x | ||
| Catastrophe Reinsurance, outside rating agency bounds | x | ||
| High limit property per risk reinsurance | x | ||
| Personal lines for affluent individuals | x | x | |
| Small commercial lines | x | x | |
| Catastrophe reinsurance, within rating agency bounds | x | x | |
| Large account captive reinsurance | x | ||
| Structured quota share, requiring a risk transfer test | x | x | |
| Working layer casualty excess of loss | x | x | |
| Surplus relief quota share on cat exposed line | x | x | x |
| Middle market commercial lines work comp or commercial auto | x | x | x |
Insured’s needs are orthogonal to the marketing channel: they represent a separate set of decisions.
There are secondary goals met by insurance. For example, (Kunreuther et al. 2013) enumerate
- status quo,
- reduce anxiety about a loss,
- avoid regret in case a loss occurs,
- budget constraint,
- investment, i.e. expected losses exceed premium,
- social norms, presenting the appearance of prudence, and
- maintaining a relationship with an agent or broker.
Although these are all interesting, they will not be considered further.
Insured’s needs place constraints on the entity selling products to meet those needs. Laws, regulations, and custom dictate details of the underlying policy form and place restrictions on admissible insurers. These regulations specify product details and insurer characteristics, they are not regulations of insurers per se. Here are three common examples.
- Automobile financial responsibility laws in most states require drivers show some form of financial responsibility. The easiest form is to have car insurance issued by an insurer authorized to conduct business in the state. State law specifies required coverages and minimum limits of liability, which vary from $30,000 per accident up to $100,000 per accident. Most states maintain a residual market facility to ensure all drivers have access to insurance.
- Conforming mortgages require a homeowners policy “protect against loss or damage from fire and other hazards covered by the standard extended coverage endorsement. The coverage must provide for claims to be settled on a replacement cost basis. Extended coverage must include, at a minimum, wind, civil commotion (including rise), smoke, hail, and damages caused by an growth, vehicle, or explosion.” Policies that limit or exclude coverage from windstorm, hurricane, or hail damage are not acceptable. In addition the policy must be written by a carrier with an A.M. Best Company, Inc. Financial Strength Rating of B or better, a Demotech, Inc. Rating of A or better, or a Standard & Poor’s financial strength rating of BBB or better.
- Workers compensation laws vary by state and usually require virtually every employer to provide workers compensation insurance for all employees. Insurance can be purchased from a commercial provider authorized to conduct business in the state or a state administered residual market fund. Approved businesses are often allowed to self-insurer, either individually or as part of the group. Workers compensation benefits also vary by state and are specified precisely in regulation.
As a result of these regulations, US insurance companies meeting satisfying needs are typically licensed or admitted to write specific lines of insurance by one or more state’s regulators. They are a statutory insurance entities. They also maintain an adequate claims paying ability rating, as issued by a nationally recognized statistical rating organization (NRSRO). NRSROs are recognized by the U.S. Securities and Exchange Commission (SEC), which permits other financial firms to use their ratings for certain regulatory purposes. There are currently 10 NRSRO. A. M. Best is the most commonly quoted for insurance, followed by Standard and Poor’s, Moody’s Investors Service, and Fitch Ratings. In addition, Demotech, Inc. ratings are accepted by Fannie Mae, Freddie Mac and the HUD and as a result are acceptable to mortgage lenders. For various reasons Demotech ratings dominate the Florida homeowners insurance market.
Meeting an insured’s risk pooling needs requires the ability to credibly assure individual insureds in the pool that
- the pool can offer appropriate insurance coverage;
- they will be treated fairly and equitably relative to other insureds in the pool; and
- the pool will remain solvent and able to pay all its claims obligations.
Thus, risk pooling encompasses product design, pricing, and underwriting; objective and fair claim settlement; and the maintenance of an adequate capital buffer to absorb adverse loss experience.
If the insured also has a satisfying requirement, then insurance coverage will be prescribed by law, regulation, contract, or custom. Only the largest and most sophisticated insureds create custom, or manuscript, insurance forms. Coverage design is therefore most important in discretionary insurance purchases, such as warranty insurance or travel insurance.
Fairness and equitable treatment within the pool is an important part of an insurer’s brand image and market reputation. Insurers are aware of its importance, and emphasize it in their public’s relations and marketing material. In addition, for mandated lines, states regulators audit compliance with laws and regulations.
Financial solvency is monitored by regulators, rating agencies, agents and brokers, and, in some cases, by insureds directly. The relative importance of regulation and rating agencies varies by country. In the US statutory capital requirements are relatively low and rating agency requirements dominate. In Europe, Solvency II has created tougher regulatory requirements, though companies still typically hold 150% or more of their Solvency II required capital.
Insureds can finance low volatility risk cost efficiently using self-insurance, large deductibles or self-insured retentions, captive insurers, and risk retention groups. If the insured must also satisfy an insurance requirement, for example workers compensation, a captive is used in conjunction with admitted insurance paper. An admitted carrier issues an insurance policy in each state which the insured’s captive then reinsures. If there is no specific insurance requirement the captive can issue a policy directly, a structure seen in environmental insurance for example.
The need for custom coverage design, often including broader coverage that is available in the open market, is also cited as a reason for captive insurers. This is really a risk financing function.
Figure 6 and Table 8 summarize the cumulative effect of the insured’s combined satisfying, risk financing and risk pooling needs. Satisfying needs put constraints on the entity issuing the insurance contract; financing constraints can alter the flow of funds to divert premium to more efficient vehicles and finally risk pooling requires an assurance of fairness and a demonstration of solvency.
| Sat | RP | RF | Admitted or Licenced | Rated |
|---|---|---|---|---|
| x | x | |||
| x | x | |||
| x | x | x | x | |
| x | ||||
| x | x | x | ||
| x | x | x | ||
| x | x | x | x | x |
Managing Conflict with Capital
Three principal stakeholders interact within the Paper function: insureds, management, and Capital, which is discussed in the next section, and which bears any residual risk of the Paper insurance pool. There are inherent conflicts between the functions of insured, managers, and Capital and the market has developed different approaches to managing these conflicts depending on their relative degree (Mayers and Smith 1988) accounting for the variety of insurance structures. In additional this paper argues that insurers specialize to deliver products meeting different insured needs and this also helps explain the variety of structures seen in the market.
Turning first to conflicts, Figure 7 displays actual and potential conflicts between insureds, management and Capital in the most common organization forms: mutuals and reciprocals, stock companies and the Lloyd’s arrangement. The direct costs incurred to control incentive conflicts include negotiation, administration, information, and litigation costs. Indirect costs reflect the fact that it is generally optimal to allow management some discretion (Mayers and Smith 1988) and (Mayers2000?).
Mutuals and reciprocals merge the owner and insured function ensuring an alignment of interest. There is still potential conflict with management, and since mutual companies cannot align management interest through equity based compensation these structures are regarded as optimal when management needs minimal discretion. The structures are best suited to high-volume lines where loss data supports the creation of very detailed classification rate manuals, such as personal automobile, homeowners, and workers compensation (Mayers and Smith 1988).
In the mutual company structure insurance policies are issued by a limited liability company. The company employs management and management is directed by a board elected by insured owners. In the reciprocal, or into the insurance exchange, structure insurance policies are mutual indemnifications between insurance; there is no separate legal entity issuing policies. The reciprocal exchange is managed by a board of insured members. The board appoints an attorney in fact which performs management functions. Attorneys in fact can be owned by stock companies, for example Erie Indemnity Co. or Zurich Insurance, which owns the Farmers Exchange, and Plymouth Rock, a private stock company owning the Palisades Insurance Exchange.
At the other extreme, the Lloyd’s of London model merges the roles of Capital and management. Insurance risk bearing capacity is provided by individuals and corporate members to the underwriting syndicates. Underwriting members of the syndicates sit in Managing Agents, companies that employ the underwriting staff and handle the day-to-day running of a syndicates infrastructure and operations (Lloyds 2011). The alignment of underwriting and Capital is most useful for lines requiring significant underwriting and management discretion and a Lloyd’s is world-renowned for its ability to underwrite and accept any type of risk.
Like reciprocals, syndicate members are individually liable for their share of the insurance policies the syndicate writes. However, unlike reciprocals, syndicates can write insurance for unrelated entities.
Historically Lloyd’s managed the conflict between Capital and insured by requiring syndicate members assume unlimited liability. As Lloyd’s emerged from the difficulties caused by asbestos and environmental losses in the 1990s, unlimited liability was replaced with a limited liability structures and with the ability of corporations to become members of syndicates. As a result, today Lloyd’s manages the Capital-insured conflict largely on the basis of history of paying all claims when due since its founding in 1686: a very hard to replicate credential!
The stock insurance company structure sits between the mutual structure and Lloyd’s structure. There is a full separation between insureds, Paper managers, and Capital owners. The resulting increase in potential conflicts is offset in two ways. Capital owners can alignment the interest of management through equity-based compensation. And the structure allows management greater discretion to respond to insured needs.
Implications for Paper Structure
Paper management must control product underwriting and pricing, supporting capital structure, including reinsurance, and maintain close control over claims.
Market history has shown by far the most effective way of achieving these objectives is a traditional insurance company structure combining pricing and underwriting, capital management, and claims.
There are instances where product design, pricing, and underwriting have been separated. For example MGA program business, which is marketed to a particular affiliation, industry group or association with specialized insurance needs often disaggregated’s product design, pricing, and even underwriting from capital. The MGA controls “the pen” and combined a fronting insurance company to risk. The structures have known incentive hazards. Often the MGA participates in reinsurance to take risk away from the front the company. However, MGA business is extremely procyclical with the insurance underwriting cycle. Similarly misaligned incentives were in large part responsible for the subprime mortgage fiasco that drove the global financial crisis.
1.4.4 Market Distribution by Paper Function Organization
Table 9 show stock companies account for 61% of total premium and 59% of total surplus, mutuals 29% and 31%, and reciprocals 10% and 7%. Stock companies have higher proportionate loss reserves, reflecting legacy large commercial lines liabilities. Stock companies have almost average leverage, mutual companies below average leverage and reciprocals above average.
Table 10 reveals stock companies and mutual companies have very similar overall expense ratios of 37.0% and 37.8% respectively. Reciprocal exchanges have significantly lower total expenses of 32%.
| Organizational Form | Net EP | Percent Total | Surplus | Percent Total | Total Assets | Percent Total | Loss Reserves | Percent Total | Lever-age |
|---|---|---|---|---|---|---|---|---|---|
| Stock | 324.5 | 61% | 437.2 | 59% | 1,258.2 | 66% | 448.5 | 71% | 0.74 |
| Mutual | 156.2 | 29% | 228.3 | 31% | 513.1 | 27% | 151.2 | 24% | 0.68 |
| Lloyds | 0.3 | 0% | 0.4 | 0% | 1.0 | 0% | 0.4 | 0% | 0.79 |
| Reciprocal | 51.0 | 10% | 55.1 | 7% | 125.5 | 7% | 33.8 | 5% | 0.93 |
| Other | 1.5 | 0% | 14.0 | 2% | 22.2 | 1% | 2.3 | 0% | 0.11 |
| Industry | 533.5 | 100% | 735.0 | 100% | 1,920.1 | 100% | 636.2 | 100% | 0.73 |
| Type of Company | Customer | Paper | Claims | Sum |
|---|---|---|---|---|
| Stock | 17.8% | 7.9% | 11.4% | 37.0% |
| Mutual | 20.0% | 5.7% | 12.1% | 37.8% |
| Lloyds | 19.0% | 6.6% | 8.8% | 34.5% |
| Reciprocal | 15.1% | 6.1% | 10.9% | 32.0% |
| Other | 3.9% | 1.2% | 3.1% | 8.2% |
| Industry | 18.1% | 7.0% | 11.5% | 36.7% |
Note Lloyds represents different than LoL; included for totaling.
All tables from MILDENHALL - Expense Analysis by Type of Company AMB IEE.xlsx Analysis 1 tab.
1.5 Value and Organization of the Capital Function
1.5.1 Description of the Capital Function
The Capital function of risk bearing ensures adequate, liquid financial resources are available to guarantee claims paying ability for the risk pool, especially in adverse loss scenarios. The Paper function is responsible for decisions about the amount and form of capital. The Capital function is the actual provision of the resources. It is a purely financial function. Capital is provided to Paper in a number of forms:
- Reinsurance, including traditional, collateralized
- Debt, in the form of surplus notes
- Equity capital
- Insurance linked securities such as cat bonds and industry loss warranties
- Hybrid securities
(Paper is resp. for investing and hence the liquid part?)
For US property-casualty insurers Capital costs account for XX to YY percent of total expenses.
The Capital function includes the cost of the financial resources required to maintain insurer solvency compliant with the regulatory and rating agency standards, and hence maintaining an effective and efficient risk pool for insureds.
Capital function expenses are estimated separately for debt, reinsurance and equity as follows.
- Debt use is a very small proportion of capital and is ignored.
- The net cost of reinsurance by line is estimated as a multi-year average of the difference between the direct and net IEE pretax profit or loss from excluding all investment gain. It is averaged over a number of years
- The cost of equity capital is estimated based on a number of studies and the current industry surplus leverage ratio.
Capital function expenses cannot all be computed by line of business, unlike the other three components. The reinsurance component can be computed by line in theory, but the IEE does not split non-proportional assumed reinsurance by line, so a true net cost is not possible. Primary insurers however rarely have material non-affiliated, non-proportional assumed operations so this is not a serious deficiency. Equity capital is a shared resource and so there is no canonical allocation; in theory all capital stands behind all policies. Capital will not be allocated by line; instead its cost will only be reported in aggregate.
Capital function expenses are an external cost of financing.
The next three subsections discuss the value of debt, reinsurance and equity capital in detail.
1.5.2 The Value of Debt Capital
US Property-casualty insurers can use a special form of subordinated debt called surplus notes as equity. However, the industry makes relatively little use of surplus notes. In 2016 the US PC industry debt to total capital ratio was only 1.7 percent, stock companies 1.2 percent and mutual companies 1.8 percent. Reciprocals used 5.0 percent surplus notes. As a result no specific adjustment is made for debt in the following analysis.
1.5.3 The Value of Equity Capital
Need the math with PV of loss and the magically disappearing taxes!
Several studies have attempted to estimate the cost of equity capital for property-casualty insurers including (Cummins and Phillips 2005) and (Cummins et al. 2010) These studies produce a broad range of estimates from 10 percent to 12 percent using a CAPM beta model to 17 to 18 percent using the Fama-French three factor model. Cummins and Weiss (2013) select a 13.2 percent cost of capital.
Historically the US property-casualty industry has made far lower returns. Since 2001 the compound average ROE based on net income to average equity has been 7.3 percent, 8.0 percent since 2003 and 8.5 percent over the last five years. Including changes in unrealized gains and losses the average ROE since 2001 is 4.9 percent, 8.8 percent since 2003 and 9.3 percent over the last five years. [Include a table!]
Based on these inputs a cost of equity capital of 12.0 percent will be used, with 10 percent and 13.2 percent also shown in a sensitivity analysis.
Investors benefit from the investment spread over amounts credited in premium on policyholder provided funds, predominantly loss reserves. These are the amounts Warren Buffett famously describes as “the float”. Investors also benefit from the total investment return on investor provided funds. The investor return is after-tax and so insureds must pay income tax to return the desired after-tax investor return.
Therefore the cost of equity to insureds is computed as \(\rho E/(1-\tau) - rA\) where \(\rho=0.12\) is the cost of equity capital, \(\tau=0.156\) is the average Federal income tax rate since 2009, \(E\) is the average equity, equal to $697.6 billion in 2016, \(r\) is the total return on invested assets and \(A\) is average invested assets, equal to $1,559.5 billion in 2016. The total return on invested assets includes net investment income, realized gains and losses and change in unrealized gain and loss, all on a pre-tax basis. Since 2001 \(r\) has ranged from -5.2 percent in 2001 to 7.3 percent in 2003, with an all year average of 3.8 percent, 4.5 percent since 2003 and 4.8 percent over the last five years.
| Cost of Capital \(\rho\) | 10.0% | 12.0% | 13.2% |
|---|---|---|---|
| \(r=0.038\) | 3.8% | 6.5% | 8.2% |
| \(r=0.045\) | 2.1% | 4.9% | 6.5% |
The table above shows the implied cost of equity capital as a percentage of estimated 2016 direct earned premium of $602.6 billion. The calculations below are based on a selected cost of 5 percent.
1.5.4 The Value of Reinsurance Capital
At a high level the ex post the net underwriting cost of reinsurance by line can be computed as the difference between the direct underwriting profit and the net underwriting profit from the IEE. Averaging these realized costs over a number of years will produce an actuarial estimate of the prospective cost. The rest of the sub-section works to make this high-level description more precise. First the accounting is clarified. Then the method is applied to historical IEE data to produce estimated costs. Finally shortcomings of the method are discussed.
The ex post underwriting income cost of reinsurance to an insurer is the difference between direct pretax profit or loss, excluding all investment gain and net pretax profit or loss excluding all investment gain. Both views are available in the IEE, but there is a quirk in exactly how some reinsurance is reported.
Insurance companies can cede or assume reinsurance to or from other insurers. In the IEE proportional reinsurance, both assumed and ceded, is included within the net results for the appropriate statutory line of business. Non-proportional reinsurance ceded is also included in the net result for each line. However, non-proportional reinsurance assumed becomes a new line in the net IEE. The reason is that a non-proportional treaty can cover multiple lines of business with a single, indivisible premium and so there is no canonical allocation back to line. As a result of this treatment, it is impossible to get a true net result by line.
To make the accounting precise first recall that the net result is direct plus assumed minus ceded. Next, let \(D_i\) be the direct underwriting result for line \(i\in I\), \(I\) the set of lines written directly, and let \(D=\sum_{i\in I} D_i\) be the total direct underwriting result. And let \(N_i\) be the net result and \(N=\sum_{i\in I} N_i + N_a\) be the total net underwriting result, where in addition to the direct lines \(i\in I\) the total includes the result \(N_a\) of non-proportional reinsurance assumed. Therefore \(D_i-N_i\) represents the ex post net cost of reinsurance for line \(i\), including any cost or benefit from proportional business assumed but excluding possible benefit from non-proportional reinsurance assumed.
Thus the total ex post cost of reinsurance can be estimated as \(D-N = \sum_{i\in I} (D_i-N_i) - N_a\). Usually \(-N_a<0\) is a negative expense and a company’s reinsurance assumed operation acts to lower the net cost of reinsurance. However for other lines \(D_i-N_i > 0\) and there is a cost to the insurer of using the risk pooling services of the reinsurance market.
\(D_i-N_i\) combines the effect of ceded premium, a reduction in expenses through a ceding commission, and a reduction in losses and loss adjustment expenses. It would be possible to analyze Paper and Claim function expenses on a net basis. However, since reinsurance is a part of the Capital function its full net cost should reside within Capital, and the full direct cost of customer acquisition and administration, and of loss adjustment, should sit in the Customer and Claim categories respectively. Therefore the analysis uses direct expenses and reflects reinsurance through its net impact on Capital costs. As far as I am aware this represents a new analysis of reinsurance costs.
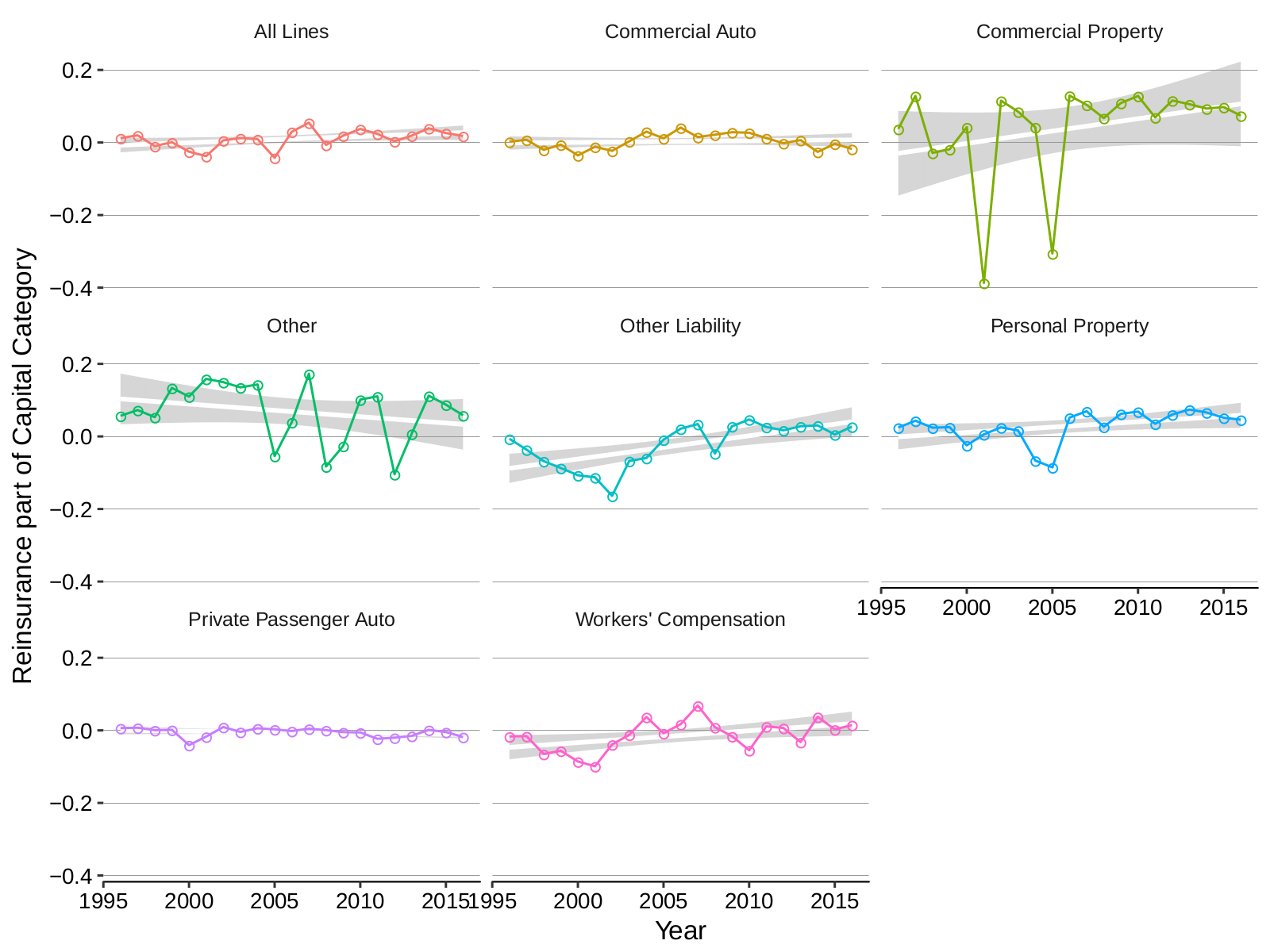
So far estimated reinsurance costs \(D_i-N_i\) are ex post, not a priori: they are experience and not a rate. They include a random component from the occurrence or non-occurrence of reinsured losses. Since reinsurance is usually purchased to protect against large, infrequent, or catastrophic losses the net cost of reinsurance must be estimated using a long-term average. The analysis uses data since 1996 to estimate the cost of reinsurance. During this time reinsurance pricing experienced a severe soft market, from 1997 to 2000, was impacted by the World Trade Center catastrophe in 2001, and experienced Hurricane Katrina in 2005, still the largest insurance loss ever recorded. However, it also included the longest recorded gap between land-falling major hurricanes in the US from 2005 until 2017.
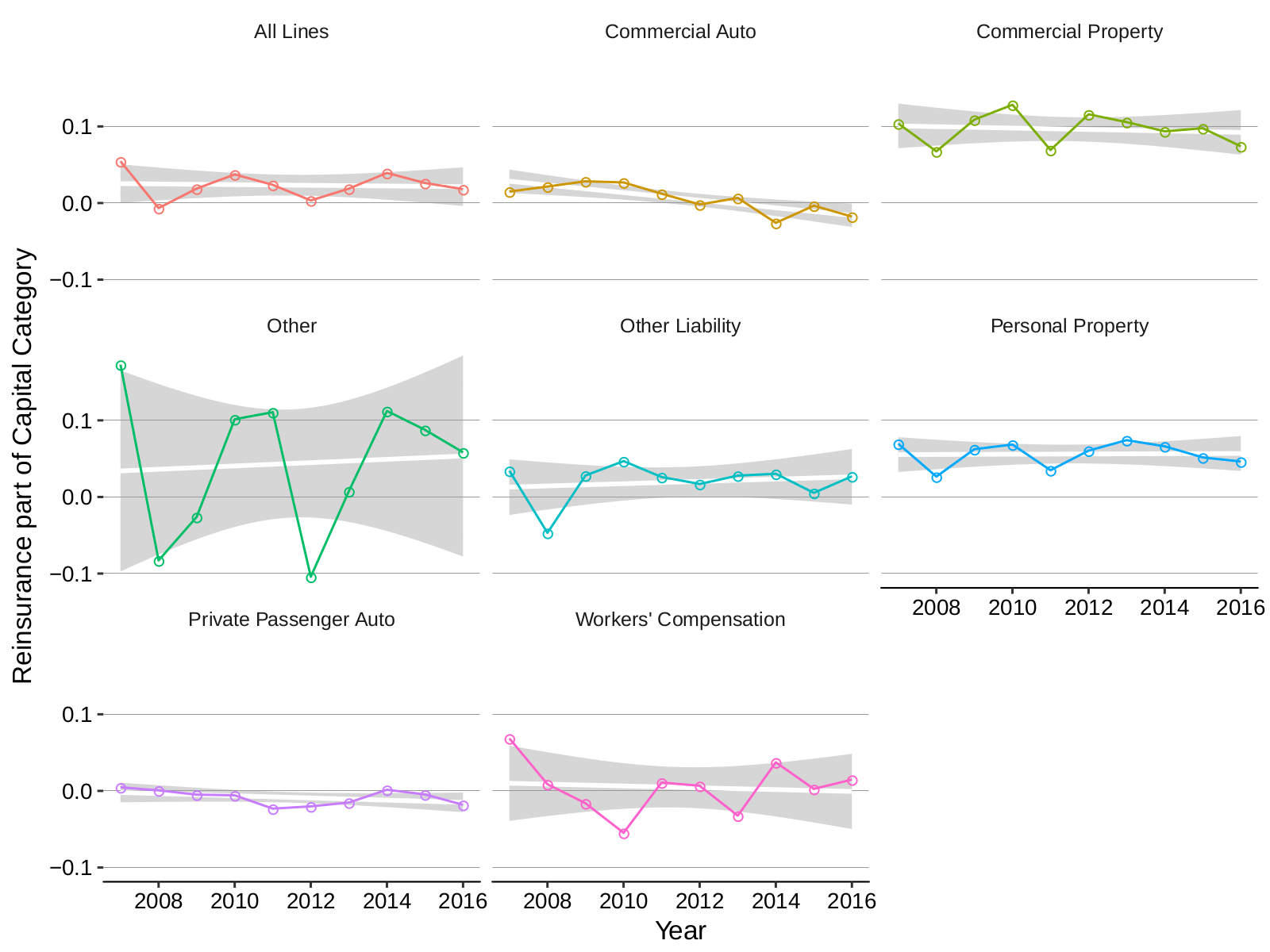
Reinsurance expenses as a percentage of direct and premiums are reported in Table 12 and Table 12. These exhibits report ex post realizations of reinsurance results and are therefore more volatile than the other expense components. The analysis by line of business reveals commercial property and personal property have the highest direct loadings. Softening in the commercial auto reinsurance market is shown by the fact the insurance expense was negative in 2014, 2015 and 2016. Private passenger auto reinsurance reflects the operation of residual market pools and is also consistently negative, i.e. an expense benefit. Table 13 shows a longer time series of direct reinsurance results by line of business, that is more suitable for estimating average costs, although results for other liability are unreliable prior to 2009. In this table assumed business is included as an offset in the Other line. The remaining lines show the net benefit of proportional reinsurance plus the cost of ceded non-proportional reinsurance. Since 1996 this net cost has been 0.0% for commercial auto, driven by extremely soft pricing from the late 1990s that emerged between 1998 and 2003; 4.4% for commercial property; 3.7% for personal property; a benefit of -0.6% for private passenger auto, and a benefit of -1.2% for workers compensation, also driven by extremely soft pricing from the late 1990s and severe losses in the World Trade Center catastrophe.
In Table 14 the DIRECT column shows the difference between direct underwriting and net underwriting results (i.e. \(\sum_{i\in I}(D_i-N_I)\)) as a percentage of direct earned premium since 1996 across all lines. It is computed by line and reflects proportional business ceded and assumed as well as non-proportional business ceded. The ASSUMED column shows the underwriting result of non-proportional reinsurance assumed (i.e. \(N_a\)) as a percentage of total earned premium. If ASSUMED is negative then reinsurance assumed business is a negative expense, i.e. acts as an offset to ceded reinsurance expenses. The NET COST column is the sum of DIRECT and ASSUMED; it shows the net cost to the insurer of all reinsurance activities. The table reveals several points.
- Reinsurance has a clear loss smoothing effect in severe catastrophe years, with a direct expense benefit of 6.2% in 2001 and 9.2% in 2005. However, these benefits were somewhat offset by assumed reinsurance losses of 3.1% and 3.0% respectively.
- The soft reinsurance market of the late 1990s is clear, with a direct reinsurance benefit in 1998, 1999 and 2000.
- More rational reinsurance pricing since 2002, as the reinsurance market became dominated by professional reinsurers, is also evident. Direct reinsurance was a net expense for all years after 2002, except for Katrina-driven 2005.
- Overall (excluding the issues with other liability prior to 2009) direct reinsurance expenses were 1.0% of direct earned premium on average since 1996. Over the last 10 years since 2007, a period with no significant reinsured catastrophes, direct reinsurance expenses average 2.6% of direct earned premium. Since 2002, the professional reinsurance market period, direct reinsurance expenses averaged 1.8% of direct earned premium.
- Insurance company assumed reinsurance operations have not performed well over the long-run. Since 1996 they have averaged an expense of 0.2% of direct earned premium per year, i.e. assumed operations increased net reinsurance expenses by 0.2%. Assumed reinsurance did not recover as quickly as the professional market after the soft market of the late 1990s, producing a net loss every year from 1996 through 2005. Over the last 10 years since 2007 assumed reinsurance produce an average benefit of 0.3%, i.e. assumed operations lowered net reinsurance expenses by 0.3%. Since 2002 assumed reinsurance expenses averaged 0.1% of direct earned premium.
- Reinsurance costs in the 2002-2016 professional market period, which includes Katrina in 2005 and very poor severe weather losses in 2010 and 2011, are 1.9% of direct earned premium, including the effect of assumed reinsurance operations.
| LINE | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|---|---|---|---|
| All Lines | 0.055 | -0.007 | 0.019 | 0.037 | 0.024 | 0.003 | 0.019 | 0.039 | 0.026 | 0.018 |
| Commercial Auto | 0.015 | 0.022 | 0.028 | 0.027 | 0.012 | -0.002 | 0.007 | -0.026 | -0.003 | -0.018 |
| Commercial Property | 0.104 | 0.067 | 0.109 | 0.128 | 0.069 | 0.116 | 0.106 | 0.094 | 0.098 | 0.074 |
| Other | 0.173 | -0.083 | -0.026 | 0.101 | 0.111 | -0.104 | 0.007 | 0.112 | 0.088 | 0.058 |
| Other Liability | 0.034 | -0.047 | 0.028 | 0.047 | 0.026 | 0.017 | 0.028 | 0.030 | 0.005 | 0.027 |
| Personal Property | 0.070 | 0.027 | 0.062 | 0.068 | 0.035 | 0.061 | 0.074 | 0.066 | 0.052 | 0.046 |
| Private Passenger Auto | 0.005 | 0.001 | -0.005 | -0.006 | -0.023 | -0.020 | -0.015 | 0.002 | -0.005 | -0.018 |
| Workers’ Compensation | 0.069 | 0.009 | -0.016 | -0.055 | 0.011 | 0.007 | -0.032 | 0.037 | 0.003 | 0.015 |
| Year | All Lines | Comm-ercial Auto | Comm-ercial Property | Other | Other Liability | Personal Property | Private Pass-enger Auto | Workers’ Comp-ensation |
|---|---|---|---|---|---|---|---|---|
| 1996 | 0.012 | 0.002 | 0.037 | 0.057 | -0.006 | 0.024 | 0.006 | -0.017 |
| 1997 | 0.020 | 0.008 | 0.129 | 0.073 | -0.036 | 0.043 | 0.007 | -0.016 |
| 1998 | -0.010 | -0.020 | -0.029 | 0.053 | -0.068 | 0.024 | 0.001 | -0.065 |
| 1999 | 0.001 | -0.006 | -0.018 | 0.134 | -0.087 | 0.026 | 0.001 | -0.056 |
| 2000 | -0.025 | -0.036 | 0.042 | 0.110 | -0.107 | -0.024 | -0.041 | -0.086 |
| 2001 | -0.038 | -0.012 | -0.387 | 0.159 | -0.113 | 0.006 | -0.017 | -0.099 |
| 2002 | 0.006 | -0.023 | 0.115 | 0.150 | -0.164 | 0.025 | 0.009 | -0.039 |
| 2003 | 0.012 | 0.003 | 0.085 | 0.135 | -0.068 | 0.016 | -0.004 | -0.012 |
| 2004 | 0.009 | 0.030 | 0.042 | 0.143 | -0.059 | -0.066 | 0.006 | 0.037 |
| 2005 | -0.042 | 0.012 | -0.306 | -0.054 | -0.009 | -0.085 | 0.003 | -0.008 |
| 2006 | 0.030 | 0.041 | 0.129 | 0.039 | 0.021 | 0.052 | -0.002 | 0.017 |
| 2007 | 0.055 | 0.015 | 0.104 | 0.173 | 0.034 | 0.070 | 0.005 | 0.069 |
| 2008 | -0.007 | 0.022 | 0.067 | -0.083 | -0.047 | 0.027 | 0.001 | 0.009 |
| 2009 | 0.019 | 0.028 | 0.109 | -0.026 | 0.028 | 0.062 | -0.005 | -0.016 |
| 2010 | 0.037 | 0.027 | 0.128 | 0.101 | 0.047 | 0.068 | -0.006 | -0.055 |
| 2011 | 0.024 | 0.012 | 0.069 | 0.111 | 0.026 | 0.035 | -0.023 | 0.011 |
| 2012 | 0.003 | -0.002 | 0.116 | -0.104 | 0.017 | 0.061 | -0.020 | 0.007 |
| 2013 | 0.019 | 0.007 | 0.106 | 0.007 | 0.028 | 0.074 | -0.015 | -0.032 |
| 2014 | 0.039 | -0.026 | 0.094 | 0.112 | 0.030 | 0.066 | 0.002 | 0.037 |
| 2015 | 0.026 | -0.003 | 0.098 | 0.088 | 0.005 | 0.052 | -0.005 | 0.003 |
| 2016 | 0.018 | -0.018 | 0.074 | 0.058 | 0.027 | 0.046 | -0.018 | 0.015 |
| Average | 0.012 | 0.004 | 0.053 | 0.064 | -0.015 | 0.035 | -0.006 | -0.008 |
| Year | Direct | Assumed | Net Cost |
|---|---|---|---|
| 1996 | 0.009 | 0.003 | 0.012 |
| 1997 | 0.018 | 0.002 | 0.020 |
| 1998 | -0.012 | 0.002 | -0.010 |
| 1999 | -0.010 | 0.011 | 0.001 |
| 2000 | -0.033 | 0.008 | -0.025 |
| 2001 | -0.065 | 0.028 | -0.038 |
| 2002 | -0.005 | 0.011 | 0.006 |
| 2003 | 0.009 | 0.003 | 0.012 |
| 2004 | 0.003 | 0.007 | 0.009 |
| 2005 | -0.064 | 0.021 | -0.042 |
| 2006 | 0.031 | -0.001 | 0.030 |
| 2007 | 0.053 | 0.001 | 0.055 |
| 2008 | -0.009 | 0.002 | -0.007 |
| 2009 | 0.025 | -0.007 | 0.019 |
| 2010 | 0.041 | -0.003 | 0.037 |
| 2011 | 0.020 | 0.004 | 0.024 |
| 2012 | 0.008 | -0.004 | 0.003 |
| 2013 | 0.023 | -0.005 | 0.019 |
| 2014 | 0.038 | 0.001 | 0.039 |
| 2015 | 0.030 | -0.004 | 0.026 |
| 2016 | 0.021 | -0.003 | 0.018 |
| 2999 | 0.009 | 0.003 | 0.012 |
| Average | 0.010 | 0.002 | 0.013 |
| 2007-2016 | 0.026 | -0.003 | 0.023 |
| 2002-2016 | 0.018 | 0.001 | 0.019 |
1.5.5 Organization of the Capital Function
It is management’s responsibility to determine Paper’s capital needs and to design and implement an optimal capital structure using a mix of market instruments. It is also Paper management’s function to invest the resulting assets. The Capital function represents the actual provision of the capital resources.
Probably the most important capital structure management decision is the proportion of capital to “out-source” using reinsurance. Currently US companies use an average mix of 23% reinsurance and 77% and balance sheet capital. Variation in the use of reinsurance as a proportion of total risk bearing capacity is the most obvious manifestation of different organizations of Capital. However, this is essentially unobservable. One commonly used proxy is the net proportion of premium ceded to reinsurers, which is easily observed.
Affiliates vs. non-affiliates. Schedule F analysis. Pended.
1.6 Value and Organization of the Claims Function
1.6.1 Description of the Claims Function
The Claim function provides the real financial service of adjusting, settling and paying claims includes the following.
- Receiving first notice of loss, often via a 24/7 call center.
- Coverage verification.
- Claim investigation.
- Performing the contractual obligation to defend an insured. For many liability lines of business loss adjustment expenses are a substantial proportion of indemnity payments. However, they represent real services to the insured who otherwise would have to arrange for their own defense. Insurers by specializing in the settlement of such claims can create a real competitive advantage as well as a cost advantage through specialization, scale, and preferential service provider agreements.
- Litigation and legal services.
- Fraud detection and management, special investigation unit (SIU). For example using data mining to monitor for suspicious patterns of doctors and lawyers working together.
- Subrogation.
- Medical treatment and medical bill review.
- Arbitration.
- Offering assistance to first-party claimants ranging from referrals, preferred service provider networks through direct management of remediation (e.g. surety).
- Claims payment.
- Risk management services, by providing feedback to risk engineering and loss prevention teams.
For US property-casualty insurers Claims costs account for nearly PP percent of total expenses.
Claims function activities can be performed by out-sourced adjusters, call Third Party Administrators, but close integration with Paper is by far the most common form.
Claim function expenses are computed from the IEE by combining
- Defense and cost containment expenses and
- Adjusting and other expenses.
Claim function expenses can be computed by line of business.
The claim department is often the largest single department in an insurance company. Direct people costs, including salary, benefits and payroll taxes, account for 42 percent of claims expenses. Claims operations are technology-heavy, managing a large volume of transactions. Claims also incurs management overhead expenses.
1.6.2 Value of the Claims Function
Claim function expenses as a percentage of direct and premiums are shown in Table 15 and Table 15. Across all lines claim expenses have decreased 1.2 percentage points since 2009, from 12.3% to 11.1%. Claim function expenses vary significantly by line of business, exceeding 20% of direct earned premium in Other Liability. In general liability lines have higher expense ratios than first party property lines. Personal property are nearly 2 percentage points higher than commercial property driven by lower average claim severity, and the lower deductibles. Personal auto and commercial auto have very similar claim expense ratios.
| LINE | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|---|---|---|---|
| All Lines | 0.110 | 0.115 | 0.123 | 0.118 | 0.118 | 0.117 | 0.113 | 0.111 | 0.112 | 0.111 |
| Commercial Auto | 0.109 | 0.110 | 0.113 | 0.115 | 0.111 | 0.121 | 0.123 | 0.121 | 0.127 | 0.127 |
| Commercial Property | 0.056 | 0.055 | 0.083 | 0.056 | 0.068 | 0.060 | 0.054 | 0.055 | 0.054 | 0.057 |
| Other | 0.039 | 0.045 | 0.055 | 0.062 | 0.046 | 0.049 | 0.044 | 0.033 | 0.037 | 0.039 |
| Other Liability | 0.206 | 0.206 | 0.225 | 0.213 | 0.210 | 0.206 | 0.200 | 0.197 | 0.194 | 0.187 |
| Personal Property | 0.082 | 0.104 | 0.102 | 0.091 | 0.101 | 0.092 | 0.082 | 0.082 | 0.083 | 0.082 |
| Private Passenger Auto | 0.117 | 0.115 | 0.120 | 0.119 | 0.118 | 0.124 | 0.123 | 0.120 | 0.120 | 0.119 |
| Workers’ Compensation | 0.100 | 0.131 | 0.144 | 0.155 | 0.161 | 0.137 | 0.134 | 0.135 | 0.134 | 0.137 |
1.6.3 Organization of the Claim Function
Claims adjusting is a discrete activity within an insurance company. However, there are several reasons why it is generally regarded as a core insurer function.
- It represents the actual delivery of the insurance product to insureds, and so successful management of claim adjustment is critical to an insurer maintaining its reputation in the market. Different companies can take different views of the claim settlement process depending on the marketing and customer base. For some, settlement is simply payment of the loss. For others, defense of lawsuits is critical – for example commercial umbrella policies. For first party claims insurers may see their role as more than simply providing financial assistance, extending it to guidance as the insured recovers from a loss, possibly even delivering repair services directly. These different approaches to claim settlement are an important part of an insurer’s brand.
- First party claims put the insured in direct conflict with their insurer creating a need for subtle and nuanced claim handling. FINTECH
- Claim adjusting is very manually intensive, and claims departments are often the largest department within an insurer. It is unusual for an organization to outsource such a material function.
- Constant vigilance is required to detect and mitigate fraud.
- Contracting with external claim service providers is difficult. Cost-plus contracts incentivize overpayment of losses. Fixed cost contracts can lead to inadequate effort being applied to cost-containment, again resulting in the over payment of losses. Only a stakeholder is positioned to balance claims adjusting effort to assure a fair settlement for insurers and claimants and, simultaneously, to assure claims are not overpaid. PICARD papers.
Nonetheless, disaggregated claims adjusting is observed in certain segments of the insurance market. Sophisticated, large, and largely self-insured accounts often separate claim adjusting from risk bearing, using a third-party administrator for claims while retaining risk or sharing it with an insurer. In these instances there is essentially no underwriting, since the entity is covering its own risks. From the insured’s perspective there it is simply a choice between outsource providers: use the insurer’s integrated claims services or and third-party administrator. Either way the insured is exposed to the contracting and monitoring problems inherent in separating claim payment from claims administration.
To the extent insurers participate on a risk alongside the sponsoring entity, the prevalence and acceptance of TPA claims administration tend to run procyclically with the insurance cycle, being more prevalent during soft markets. The first sign of a hard market in large accounts business is an edict of no more TPAs.
1.7 Characterization, Management and Operation of a Traditional Insurer
This section combines results from the previous four sections to report total expenses excluding the cost of equity capital and then including it. It then summarizes the what the data tells us about why the insurance stack has the its current functional organization.
1.7.1 Value of Customer, Paper, Reinsurance and Claim Combined
Combined customer, paper, reinsurance and claim category expenses (i.e excluding the cost of equity capital) as a percent of direct earned premium are shown in Table 16 and Figure 11. These reveal combined expenses, excluding the cost of capital, of between 40.1% in 2009 and 43.1% in 2010.
Table 17 shows the eight year average is 41.1% across these four functions. Private passenger auto has the lowest average combined expense ratio at 35.5%. Personal property expenses average 43.7%, over three points lower than commercial property at 47%. Personal property benefits from lower paper costs, reflecting its higher volume, and lower reinsurance costs, somewhat offset by higher claim expenses. Other liability has the highest combined expenses of 52.2% driven by 20.4% claim expenses.
| Line | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|---|---|
| All Lines | 0.401 | 0.431 | 0.419 | 0.395 | 0.408 | 0.422 | 0.412 | 0.402 |
| Commercial Auto | 0.464 | 0.445 | 0.431 | 0.428 | 0.440 | 0.397 | 0.424 | 0.397 |
| Commercial Property | 0.495 | 0.495 | 0.441 | 0.485 | 0.482 | 0.460 | 0.461 | 0.448 |
| Other | 0.198 | 0.415 | 0.440 | 0.196 | 0.297 | 0.419 | 0.404 | 0.385 |
| Other Liability | 0.527 | 0.558 | 0.527 | 0.515 | 0.528 | 0.512 | 0.497 | 0.517 |
| Personal Property | 0.453 | 0.455 | 0.428 | 0.447 | 0.453 | 0.440 | 0.421 | 0.409 |
| Private Passenger Auto | 0.361 | 0.359 | 0.340 | 0.352 | 0.358 | 0.363 | 0.363 | 0.341 |
| Workers’ Compensation | 0.402 | 0.397 | 0.472 | 0.433 | 0.374 | 0.444 | 0.397 | 0.421 |
| Line | Customer | Paper | Re | Claim | Combined |
|---|---|---|---|---|---|
| All Lines | 0.187 | 0.084 | 0.023 | 0.115 | 0.409 |
| Commercial Auto | 0.205 | 0.095 | 0.005 | 0.118 | 0.424 |
| Commercial Property | 0.211 | 0.093 | 0.096 | 0.060 | 0.460 |
| Other | 0.182 | 0.093 | 0.043 | 0.045 | 0.362 |
| Other Liability | 0.203 | 0.086 | 0.019 | 0.204 | 0.512 |
| Personal Property | 0.211 | 0.070 | 0.056 | 0.089 | 0.426 |
| Private Passenger Auto | 0.167 | 0.076 | -0.009 | 0.119 | 0.354 |
| Workers’ Compensation | 0.167 | 0.105 | 0.006 | 0.136 | 0.414 |
1.7.2 Total Value
Table 18 summarizes all four functional insurer value components. The customer, paper and claim costs are from the All Lines average in Table 17. The reinsurance part of capital is the average net cost across all lines, and including the effect of assumed non-proportional reinsurance, between 2002 and 2016 from Table 14. The cost of equity assumption was derived in Section Section 1.5.3. According to Table 11 is it consistent with a 12% cost of equity capital and slightly less than 4.5% (4.427%) total investment return, assuming an asset to capital ratio of 2.235 and a premium to surplus ratio of 0.86 (both values from 2016), and an average effective tax rate of 15.6%.
Table 18 suggests the answer to question often asked of reinsurance brokers: what proportion of the industry risk bearing capacity is provided by reinsurance. Based on relative costs the table indicates a proportion of 19/69ths or 23.2%. The proportion will obviously vary significantly by line of business. Reinsurance costs for commercial and personal property, 4.4% and 3.7% respectively, are twice the average load indicating that closer to 40% of risk bearing capacity for these lines is provided by reinsurance. The question is sometimes asked as the ratio of reinsurance capacity to equity capacity resulting in 19/50ths or 38%. Based on the average equity of $697.6 billion underlying Table 11 this implies $265.1 billion additional equity capital would be required if no reinsurance were used. The reinsurance capital is therefore being provided at a pre-tax cost of 4.3% (11.4 / 265.1) or an after-tax cost of only 2.8% at statutory rates, compared to the assumed 12.0% cost of equity capital. This shows that reinsurance is a very efficient form of capital, helping to explain its use by the industry, but raising the question of why it is not used more extensively. (EXTEND AND EXPAND SOMEWHERE! To which the answer is reinsurance provides capital in areas where it is most efficient. A substantial proportion of equity is used to satisfy regulatory and rating agency “face capital” requirements that are inherently inefficient. This locked up capital is still at risk and behind high regulatory walls as far as an investor is concerned, and so capital is not provided by investors at a lower cost. Classic examples are the severe over capitalization of the private passenger auto market.)
| Component | Proportion of Direct Premium | Proportion of Net Premium | USD (billion) | Percent of Total |
|---|---|---|---|---|
| Customer | 0.189 | 0.215 | 113.9 | 41.3% |
| Paper | 0.085 | 0.097 | 51.2 | 18.6% |
| Reinsurance | 0.019 | 0.022 | 11.4 | 4.1% |
| Cost of equity | 0.050 | 0.057 | 30.1 | 10.9% |
| Capital | 0.069 | 0.079 | 41.6 | 15.1% |
| Claim | 0.115 | 0.131 | 69.3 | 25.1% |
| Total | 0.458 | 0.522 | 276.0 | 100.0% |
Table 19 shows the expense type composition of each component function. Overall commissions, brokerage, and allowances are the largest expense type accounting for 33.9% of total expenses. Adjusting expense, excluding insurance companies staff but including external claims adjusting services, attorney fees, and related items, accounts for 17.2% of total expenses. Overall people costs including salaries, payroll taxes and employee relations and welfare account for 17.7% of total expenses. Taxes licenses and fees account for 6.4% expenses. Within the customer category, 81.5% expenses are commissions, brokerage, and allowances and 10.7% are people costs. People costs account for almost 40% of the paper category at 23.4% of the claims category.
| Type \(\backslash\) Function | Customer | Paper | Capital | Claims | Total |
|---|---|---|---|---|---|
| Equity Capital | 72.5% | 10.9% | |||
| Reinsurance | 27.5% | 4.1% | |||
| Adjusting Expense | 0.0% | 0.0% | 68.4% | 17.2% | |
| Commission, Brokerage and Allowances | 81.5% | 1.0% | 0.1% | 33.9% | |
| People Costs | 10.7% | 39.9% | 23.4% | 17.7% | |
| Equipment, IT and Systems | 2.1% | 8.3% | 2.5% | 3.0% | |
| Advertising | 2.7% | 0.6% | 0.0% | 1.2% | |
| Taxes, licences and fees | 0.0% | 34.6% | 0.1% | 6.4% | |
| All Other | 3.0% | 15.5% | 5.6% | 5.5% | |
| Total | 41.3% | 18.6% | 15.1% | 25.1% | 100.0% |
Note: source MILDENHALL - Expense Analysis by Type of Company AMB IEE.xlsx Total US PC Stock tab.
1.7.3 Functional Organization of the Traditional Insurer
(It is the perfect vehicle to securitize insurance risk…)
While a bewildering variety of insurance and insurance-like products exist in the marketplace the overwhelming majority are provided by a traditional insurance structure with the following characteristics.
- Pools risk for multiple insureds
- May be regulated, i.e. licensed or admitted, to write business in a particular state or domicile
- Alternatively, may be non-admitted or off-shore
- Its claims paying ability is generally rated by a NRSRO
- Alternatively, it uses collateral to warrant its claims paying ability and insure its customers get appropriate credit to the insurance they buy
- Generally integrates claim adjustment services
- Integrates the management of policy form, underwriting and pricing policy, line underwriting and pricing, and capital structure
- May file its products, underwriting and pricing with relevant regulators
- Includes mechanisms to address the conflict between management and capital
These will be referred to as “Traditional Insurers”.
Thus although the four functions of an insurer, Customer, Paper, Capital and Claims, were presented separately and they can be disaggregated the most commonly observed combinations involve very tight couplings of all but Customer or of all four components in order to manage incentive and informational issues. Figure 12 summarizes the many threads that have led up to this conclusion.
Addressed below…
- Fairness between insureds: adverse selection, precision rate making = big data, AI, telematics, drones etc. better u/w and pricing, fairer claim settlement…
- Fairness with capital providers: clear information, disclosure, efficient risk shaping, etc.
- No-touch u/w and blockchain…
1.8 The Traditional Insurer in an Disruptive Technology Environment
1.8.1 Overview
Where will technology take the insurance industry? What will it look like in 5 or 10 years? The FinTech universe of startup companies is a bewildering array of small companies with clever names and fancy logos. They are often categorized and analyzed according to the potential solutions they offer: Internet of things (IOT), telematics, remote-sensing (drones), artificial intelligence, big data, financing, Blockchain, distributed trust, and so forth. An alternative categorization is problem-based. How does startup activity align to consumer problems and insurance industry problems?
There are four broad categories of problems within the industry:
- Fundamental problems of insurance product design, related to information asymmetry, morale hazard and incentives. These questions are central to the academic study of insurance. The structure of the industry has evolved solutions to these fundamental problems, sometimes over hundreds of years, that account for the functional organization we see today.
- Strategic problems: how to maximize long-term growth? What is the purpose of the industry? What does it mean to settle a claim: simple financial indemnification or a more hands-on restoration helping put the customer back on their feet post accident? Fundamentally is the industry’s principle concern for risk management or risk transfer? For example, in relation to cyber risk, should the industry sell an indemnity product of should it think more broadly about risk management advice in the model of engineered commercial property inspection and underwriting? As part of risk management, what level of paternalism should the industry show its customers, e.g. providing health, driving and other behavioral nudges?
- Business process problems addressing efficient implementations of solutions to the fundamental and strategic problems. For example, determining the most efficient mechanism to deliver sales, marketing and distribution, customer servicing, and claims settlement.
- Regulation and rating agency related realities and constraints. Fin tech can take a high-handed approach to regulation (economist article about flouting the rules) assuming that customer demand for a superior product will lead legislators to change the regulations. Given the special place of insurance in the economy, its role in protecting innocent, injured third parties, ensuring contractual performance, and protecting collateral, insurance regulation is perhaps more useful and will prove more durable than ad hoc legacy regulation of other industries. There are many commonalities of insurance regulation in different countries suggesting it serves a fundamental purpose. Don’t expect regulation to go away anytime soon!
Each is reviewed within the context of FinTech solutions. These are broadly:
- Hardware: IoT devices, cloud computing capabilities (massive, distributed, cheap and on-demand), mobile, location-aware, , wearable devices, drones, micro-satellites and other remote sensing, voice synthesis and recognition (Alexa, Siri), facial recognition;
- Data: Internet of Things (IoT) feeds, especially home monitoring IoT; driving telematics feeds; social media and other Big Data behavioral data sources
- Software: (aka analytics, and formally algorithms and implementations) predictive modeling, artificial intelligence (AI), neural networks and deep learning, propensity analysis, price elasticity modeling, voice and image recognition models;
- Financing: peer-to-peer (P2P), alternative capital, insurance linked securities (ILS) such as catastrophe (cat) bonds and industry loss warranties (ILW); collateralized reinsurance
- Trust: verification of private information in a public manner; shared databases and single source of the truth; primarily implemented using Blockchain distributed ledger technology (DLT) using cryptography, hashes, public key encryption and related technologies.
There are also new FinTech related risks to consumers demanding an industry response:
- Cyber risk
- Sharing economy coverage gaps
- Gig economy coverage gaps
These are generally covered within a discussion of FinTech’s impact on insurance.
Figure 13 shows schematically how these needs, capabilities and new risks interact.
This section addresses FinTech without reference to incumbent winners or losers. No attempt is made to discuss how incumbents should react to challengers, nor how they should organize their responses. These are important strategic questions beyond the scope of the paper.
Globally there is a frenzy of startup activity. Literally hundreds of companies are being formed on all continents, but especially in the US and China. It is a Sisyphean task to attempt to quantify and categorize them, and any effort to do so is necessarily ephemeral. This analysis aims at a more durable conceptual analysis. Updates on startups are available on-line from sites and services such as CBInsights, https://www.cbinsights.com/, and Mattermark, https://mattermark.com/.
Even a cursory analysis of the space reveals a substantial proportion of startup activity is aligned with the Customer function. Aon Benfield (2016) identifies 148 of 228 or 65% of startups in the Customer function. These companies are providing services to help customer education, needs analysis, acquisition, and intermediating risk transfer. Their efforts are global, with startups in nearly 30 countries and about 30 percent of new investment occurring outside the U.S.
Almost every start-up is leveraging data and analytics in some way: from using big data to better understand customer needs and make context-appropriate coverage recommendations to helping insurers use the same information to optimally segment and price the risk universe; from real-time location aware risk monitoring to fraud detection for more efficient claims handling. Data is clearly emerging as an important factor of production, complimenting capital and labor. The Economist recently claimed data has replaced oil as the world’s most valuable resource.
Technology continues to enable Big Data solutions, offering greater insights into human behavior. In fact there is a technology virtuous circle: technology enables a new product through cheap computing power and costless distribution, as the new product gains acceptance and uses in the market it throws off valuable data streams that can then be captured, and used to enhance the original product. Property casualty insurers have proven adept at understanding behavior from external data, for example through the well-known use of credit information. and the industry can be proud of its leadership in this area. But insurers are increasingly facing long-term trends that are behavior driven, and many insurance products, especially long-duration life insurance contracts, must understand how to shape and alter these behavioral trends. The cutting edge today is to influence behavior in the long-term in order to control and direct trends, rather than merely being a neutral by-stander. Again, start-ups are rising to the challenge, especially in health and life-sytle, with the rising popularity of wearable fitness devices, for example.
Since 2008 Blockchain technology (Nakamoto 2008) has emerged as a miracle solution in search of new problems.
In order to provide enough information about FinTech activity that the reader builds some interiority into their methods and processes Appendix Section 1.11 reproduces dozens startup narratives or elevator pitches. These center around six pillars.
- Use of technology to simplify the sales process for customers. Clearly the start-up universe feels the traditional agent or broker relationship can be improved as a mechanism to deliver needs analysis, coverage and price comparison information, particularly for personal lines or small commercial, and that an on-line self-service model is the way to go. The complexity with insurance products, coverage details and coordination, and the claim settlement process all need to be tamed. This is particularly true for younger consumers.
- Peer-to-peer insurance exchanges. These exchanges offer the promise of lower cost, through economies of purchasing or better risk selection between peers known to one-another. There is a clear challenge to the legacy industry to prove that, in fact, utilizing Big Data and sophisticated predictive modeling produces better results than self-selected groups of individuals.
- Just-in-time and mini-coverage for specific items.
- General dissatisfaction with health insurance, especially in service provision and billing. The health industry in the U.S. is more than an order of magnitude bigger than the property casualty industry. It has struggled for decades with costs that outstrip general inflation and is an aspirational target for start-ups who “want to make the world a better place.” Health insurance is a huge topic; far larger than property casualty insurance, but is beyond the scope of the paper.
- Influencing behavior – another broad topic related to the strategic question of how the industry sees its role: risk manager or more narrowly as a risk transfer portal.
- Use of Blockchain technology to improve the insurance process. This pillar is has only emerged as a force in insurance over the last two to three years. The Blockchain Industry Initiative (B3i) was incepted in 2016 and now includes an list of 37 global insurers, reinsurers and brokers including Aon, Willis and Marsh, AIG, Chubb, Allianz, Generali, Liberty Mutual, Zurich, Swiss Re and Munich Re.
The rest of the section is organized as follows.
1.8.2 Disruptive and Sustaining Innovation
Disruptive innovation is a concept introduced by Christensen (1997). Christensen differentiated sustaining innovations from disrupting ones. Sustaining innovations are customer-driven incremental changes to an existing product to maintain a competitive advantage. Think next year’s auto models. Recognizable products, but improved and appealing to a segment of customers. Christensen suggested, however, that over time the process of sustaining innovations would out-strip the needs of the average customer and leave the producer vulnerable to lower-quality products picking off less demanding customers.
A new “disrupting” innovation aimed at these low-end customers would generally be dismissed by the entrenched legacy producer: it is a clearly inferior product, it is not aimed at the “best” customers, who drive higher-margin product innovation at the top of the market. The disrupter is ignored by the incumbent and gains a foothold.
What happens next depends on how the innovation proceeds.
If, like the digital camera or smart phone, technology allows orders of magnitude improvements in capability at the same or lower cost the challenger can gradually move up the product food chain and take the business over from the incumbent.
If like eight track cartridge (so successful that if you are not old enough to remember it you won’t know what it is) the new product is only a marginal improvement and no further improvements are forthcoming the incumbent’s best strategic response is to ignore it. The challenge, obviously, is to correctly differentiate between these two outcomes!
1.8.3 Lessons from Other Industries: Disruption and De-materialization
The media industry has been disrupted by a move away from physical media to a model of on-demand streaming from massive libraries of content on a subscription basis. Users have accepted “ownership” of an invisible, ephemeral product with the advantages of massive choice, no storage costs, and low to no environmental impact over traditional physical-media owned content. The product advantages simply swamped legacy approaches, particularly for a new generation for whom they quickly became the norm: purchase of the experience not the content. This model has disrupted the markets for newspapers, music, TV, and film and through e-books, is challenging print and books.
Digital cameras offer another text-book example of a disruptive technology. Early digital cameras were not professional-ready and were not taken seriously by incumbent film manufacturers. Had incumbents asked themselves how they would have reacted had digital cameras performed at 100 or 1000 times the quality of early models, their reactions may have been different. But they did not, and by the time the products had improved to that level the war was lost.
On-line advertising is another good example of a better product winning. John Wannamaker, the department store pioneer, famously quipped “Half the money I spend on advertising is wasted; the trouble is, I don’t know which half.” On-line advertising allows buyers much more insight into which half is which, and help ensure that ads are only delivered to potential customers in the correct half! Google entered the on-line battle with a product, AdWords, which enabled very low cost product ads. They created a new market below the radar of existing players such as Yahoo, which required advertisers to spend several thousand dollars on a banner ad. Google then evolved quickly from a classic low-end disruption.
The smart phone’s success was to replace the desk top or laptop as an adequate personal computing device for most customers—customers whose predominant needs were web browsing and email. It achieved this in part by leveraging an earlier win in media through iTunes, and through encouraging a legion of app developers to fill in other customer computing needs.
Uber and Lyft provide a better, lower cost taxi service. Transparent pricing, continuously updated information on taxi arrival, no fumbling with cash, no debating the route: a clearly superior product that took legacy taxi firms by storm. Shielded by regulation, legacy firms had no expertise in responding to new competitors, and were often prohibited from competing on price. Taxis is the story of the dangers of regulation without a clear purpose producing a sclerotic industry.
A common theme in all of these examples is an overwhelmingly better product. How could instantaneous, high quality access to virtually every recorded song ever made for a small monthly fee not win out over a small collection of CDs or cassettes? Delivered through a device so addictive no one leaves home without it? Is there scope for a similar killer-app in insurance?
Another common theme is the de-materialization of the product: there is no physical newspaper, LP or CD, video or Blu-ray, or photograph. The cloud, massive decentralized computing and data centers, combined with wireless and mobile technology allow distribution of the essential product with no lasting physical manifestation. Aside from claims, insurance is already a de-materialized product.
The de-materialied tech solution is generally not a re-engineering of an existing process: it is a wholesale replacement. Think, for example, of the newspaper industry. Prior to the digital revolution newspapers built an enormously complex supply and delivery ecosystem, landing a newspaper accurately on your door step by 6:30 am each morning. Each function could have been enhanced using technology: imagine an app giving the real-time location of the newspaper delivery person. Clearly such an analysis would miss the transforming potential of technology, and it is important to stand back and ask broad, open-ended what-if questions.
1.8.4 Four Questions
Asking hypothetical questions helps envision how transformation will proceed. But it also involves a delicate balance between the possible and the conceivable.
Question 1: What do Consumers Want?
What do consumers want? Consumers do not want insurance: it is not a first-best solution! Consumers want to live in a world where the need for insurance has been managed away: a world where there are no accidents. The insurance industry has helped move the economy in this direction, for example the rate of auto related fatalities has been decreasing since records began. Frequencies of fire losses, workers compensation injuries, commercial general liability, and medical malpractice lawsuits and also experienced long-term declines over the last 20 or more years (Aon Benfield 2015). These declines have been brought about in part by the industry’s focus on risk management and safety. However, substantial residual risk remains and the nirvana of an accident free world is a dream. The prospect of driverless cars actually moves the consumer closer to no-claims nirvana. For insurers, auto represents 45 percent of global property casualty premium globally, premium that is typically associated with stable and predictable losses. One study estimated that without personal auto, loss ratio volatility for the U.S. market would have been nearly 40 percent higher for the period 1995 to 2013, and industry leverage ratios would increase by more than 30 percentage points (Aon Benfield 2014).
Question 2: What-If Underwriting Was Radically Simpler?
From the industry’s perspective it is interesting to ask: what-if insurance could be underwritten automatically given the applicant’s identity. That is, if the required underwriting information could be accessed or verified through generally accessible data sources. Concerns about privacy and security usually drown out any attempt to answer this question. However, Blockchain technology could in theory provide the necessary verifications in a safe and secure way while maintaining individual’s privacy.
Eric Raymond: “The computer should never ask the user any info that it can auto detect, copy or deduce” (from Benedict Evans)
Question 3: What-If It Was Easy for Customers to Understand Their Needs?
Discussing underwriting betrays a provider’s mindset. What about the consumer? A consumer might ask what-if I could be given a range of recommended, bindable solutions simply by disclosing my identity and authorizing data access? Recommendations customized to my personal situation, bolstered by insight into how others in my situation and act, and delivered by a trusted, neutral third-party. Recommendations bindable in the sense I could enter-into suggested coverages with a single click. And solutions not limited to traditional insurance but including behavioral nudges, self-insurance, and self-protection alternatives. Numerous start ups are attempting to provide these services.
Question 4: What-If Underwriting Capital Was More Accessible?
Finally, what-if risk owners could contract directly and costlessly, or near-costlessly, with risk bearing capital in the manner envisaged by Arrow (Kenneth J. Arrow 1996) and Borch (Borch 1962). In particular, what-if insurance costs were lowered by contractual design linking payouts to aggregate consumption as Arrow suggested? Capital market inefficiencies and the frictional cost of holding capital within an insurance entity drive a very high cost for catastrophe protection, a conundrum given the relative scale of potential catastrophe losses compared to the massive size of global capital pools, Froot and O’Connell (2008). Is there a better way to access investor capital directly?
1.9 Three Insurance Problems and Potential InsurTech Solutions
This section lays considers three insurance industry problems and shows how they align with potential InsurTech solutions.
- The use of predictive analytics enabled granular underwriting to combat the fundamental problems of adverse selection and moral hazard, which is discussed in the context of management’s responsibility to assure fairness between pool members. Relevant solutions come from the hardware, data and software components of the InsurTech stack.
- The use risk analytics and risk shaping to address management’s responsibility to assure capital adequacy, and to use capital efficiency. This addresses the interaction with regulators and rating agencies and also uses predictive analytics technologies.
- The use Blockchain and disaggregated trust to help address all four insurer problem domains, from simplifying the sales process through improved efficiency with DLT and more effective anti-fraud measures.
These problems and the associated solutions should be viewed in the context of Figure 13. The first and second problems fall into the fundamental problem domain, and are largely driven by information (hence data) issues. The third falls into the strategic and business process domains.
1.9.1 Asymmetric Information: Predictive Analytics and Granular Underwriting
Asymmetric information and ex ante moral hazard
Predictive analytics driven disruption
- within customer
- within paper
- within claims
Management’s responsibility to assure fairness between pool members using Big Data/AI granular underwriting
Mirroring an insurer’s need to understand the operations of its insureds, each individual insured in a risk pool is impacted by, and potentially concerned about, the behavior of the other insureds. This level of mutual interest is almost unique to the insurance industry.
Individual insurance are concerned that their claims will be paid, that the claims of other insurance will be overpaid and that the premium each member is charged for pool membership fairly reflects their actual loss exposure. Thus, management must be concerned not only with aggregate premium levels, which are all that is required to ensure cool solvency, but also the detailed allocation of premium to each insured.
Over the last 10 years insurance pricing has been revolutionized by the application of statistical modeling, predominantly the use of generalized linear models, and the use of non-loss underwriting information including credit scores. Looking ahead, big data offers potential insights into insurance behavioral traits which in turn reveal that loss propensity. Increased pricing sophistication will be enabled by technology and new data sources. SLIGHT LOOK AHEAD
1.9.2 Capital Market Imperfections: Risk Analytics and Risk Shaping
High frictional cost of capital, sticky capital
Management’s Responsibility to Assure Capital Adequacy: Risk Shaping and Efficiency in Risk Bearing
Insureds who purchase insurance to meet a risk pooling need must be assured of the pool’s solvency. As a result, a critical pool management question is the provision, quantity, and form of the risk of capital guaranteeing the pool’s solvency. There is a very substantial literature on measuring risk and translating risk measures into capital requirements, (Follmer et al. 2016).
In theory, in a market with no capital market imperfections there would be no need for insurers to hold capital on their balance sheets. Insurers would pool risk and pass profit cash flows directly to investors. They would be able to raise capital as needed in frictionless markets for traditional products, for which expected losses are a tiny fraction of the global capital pool. The price of capital would be unaffected by loss experience unless the experience revealed information changing underlying loss probabilities. The supply of insurance would be almost perfectly elastic, unaffected by variations in demand for insurance or insurer demand for capital. REFS
In practice, there are a series of well-known imperfections, which complicate the theoretical story. There are agency issues between management and owners, and information imperfections between insurance and management, and management and owners. In insurance markets these manifest themselves in problems of adverse selection and moral hazard. Manager inability to diversify future income streams makes them behave as though they are risk averse. Manager’s informational advantage over outside investors leads investors to “assume the worst” when management tries to raise new capital, in part explaining management solution to adverse lost on. (Journal of finance article on assuming the worst.) OTHER REFS! As a result, insurers often find external capital more costly than internal capital, further exacerbating management risk aversion (FS/FSS). As always, taxes and cost of financial distress and imperfections.
As a result managers must assemble a credible claims paying arsenal, combining on-and off-balance sheet instruments. The structure of Paper’s claims paying ability is one management’s most important responsibility.
Risk Analytics Driven Disruption: Disaggregating Capital
IC with no pool is not an IC
Carried over may be useful?
Paper represents the central service the industry provides that cannot be replicated elsewhere. Apart from its natural complexity, it is also a link with substantial regulatory protections. Insurance regulation helps protect that the promise to pay will be honored when claims are due, and generally around the world has functioned effectively. Unlike banks, where we have seen the evolution of shadow banks and regulatory arbitrage functions within so-called “shadow banks” insurance regulation has been more fit-for-purpose and has not led to significant “shadow” operations. It is hard to see the analogs of money market mutual funds (designed to circumvent regulations on the maximum interest payable on a deposit account) or the Eurodollar market (essentially to overcome exchange controls) in insurance. Thus, although regulations can be changed and can evolve over time, insurance regulation seems unlikely to be radically overhauled in the short-term and will continue to be a source of advantage to incumbents and a formidable barrier to disruptive innovators.
We have discussed the alternative capital revolution in previous editions of the Study – it is an area where the industry has embraced many new innovations over the last 25 years. And over that time period we have seen substantially lower cost of risk bearing capital brought into the industry to lower costs for customers, led by the decreases in property catastrophe reinsurance. Alternative capital allows capital to be more fungible and separated from permanent insurance paper, so it can flow into and out of markets as underlying demand ebbs and flows.
Claims adjustment services are complex and highly engineered. Numerous consulting groups provide services to fine-tune the claims process, ensuring more complex claims are handled by more experienced adjustors, understanding pain-points in the process to forestall adverse customer and claimant outcomes, and help weed out fraud and wastage in the system.
From a customer’s perspective the weak points often lie in the interaction of the parts of the chain. We have written before about the need for higher limit corporate casualty cover (so-called “giga-loss” coverage, providing cost effective risk transfer for billion dollar events). Other potential innovations, such as just in time or partial time coverage, laser cover for specific articles, microinsurance products, and cyber coverage continue to emerge. Each must cross design hurdles around potential adverse selection, customer value, insurer pricing certainty, and coverage language.
1.9.3 Onerous Underwriting and Sales: Blockchain and Disaggregated Trust
New, magical…
disaggregated trust
Micro risk pooling Provenance Smart contracts = Cat bonds
Blockchain solution… Business Imperative to Growth: Simplify Sales Process through Blockchain Databases for verification without disclosure
The Customer’s need for advice and risk intermediation services varies substantially
Personal lines customers with vanilla, statutorily or contractually driven insurance requirements generally do not demand significant pre-purchase advice. This is a classic opportunity for disruption, where the low-need, lower-end customer could be served more cheaply with a simple solution. And we have seen the industry moving towards services designed for such customers, both within the industry through the direct model, and in the Insure Tech universe with 65 percent of start-ups. Typical target customers demand greater price transparency, simpler coverage construction, and a more straightforward application process. Start-ups are delivering on all of these desires.
For more complex customers, especially in commercial lines, risk assessment and risk management needs increase substantially, and hence the demand for more comprehensive and tailored advice services increases too.
1.9.4 Evolution Ahead
The InsurTech reality facing the insurance industry is being played out in almost every sector of the economy: responding to external disruption and innovation is not unique to insurance. In many ways insurance is insulated and lucky not to have been more seriously challenged – just look at the M&A and disruption in the banking industry. Insurance industry incumbents have many strengths and a solid track record of developing new innovations, such as catastrophe modeling, predictive modeling and the use of credit scoring, and the development of alternative capital. In the short-run it is very unlikely insurance will be the next Blockbuster, DEC, or Kodak. The industry’s advantages include:
- The largest product lines are mandatory
- It operates within a challenging regulatory environment, with regulation largely rational and balanced between insurers and customers; it has not generated disruptive regulatory arbitrage in the way of banking regulation
- It is a very focused business and less susceptible to having individual customer segments picked-off
At the same time insurers have experienced disruption. Globally there has been evolution or disruption in the motor insurance market. In the US a lower-cost direct market model has gradually gained market share over the last two decades, with GEICO recently surpassing Allstate as the #2 carrier. In the UK a more radical, customer-acquisition driven disruption has shaken the market leaders and reduced the position of insurers relative to on-line aggregators. Whereas the newest top 10 auto writer in the US is Progressive, founded in 1938, in the UK three of the top 10 are newer entrants founded since 1985, when the largest, Direct Line began business (Aon Benfield 2015).
As an industry, insurers have innovated successfully, but their successes in risk modeling in some areas have paradoxically resulted in a much lower risk tolerance for newer emerging risks that cannot be modeled sufficiently well.
Today an insurer’s challenge centers around embracing, adopting and owning the best disruptive ideas, of truly surfing the wave of innovation. They must mesh their own cultures, naturally risk averse and conservative, with open, challenging thinking from innovators to address some persistent problems in the industry, notably complexity for personal lines products and high expenses across the board. A one-company, two-cultures approach, with incubators, diffuse boundaries between the firm and the start-up ecosystem has worked well in many cases. Insurers must take a more proactive stance, understanding that risk is increasingly driven by behavior and that behavior can be modified and “nudged” to reduce risk. The industry can play a part in reducing risk for society by helping educate insureds, and by providing clear, consistent and continuous feedback on risky behavior as well as incentives to act to reduce behavioral risk.
1.10 Conclusions
Mirror intro
1.11 Appendix: Start-up Narratives
In order to make InsurTech innovators more real, here are some examples of their quick-pitch narratives. These mini-stories are based on what the individual companies describe as their vision or mission. They are organized by broad theme.
Make sure you have Blockchain narratives included.
1.11.1 Better experience through education, a simpler process, or policy tracking
- answers to your many questions about costs, coverage and care
- simplifies the process of finding the most suitable medical insurance
- simplifies choosing and buying health insurance
- simplifies the experience of buying and owning personal insurance
- expert advice about health insurance to individuals and companies
- discover their coverage gaps and review solutions for their exact needs
- help users make thoughtful and well-informed decisions
- leading insurance service providers dedicated to assist you to have an adequate insurance protection for your exposure to risk.
- consumer-friendly recommendations in health insurance
- deliver a brilliant consumer experience
- an insurance education and advice platform
- truly personalized and objective recommendations on insurance plans, tailored to their individual needs and preferences for protection and cost
- a mission to reinvent the way consumers make healthcare decisions
- personal insurance management app and broker
- instant access to coverage specifics such as: specialty visits allowed, co-pays, deductibles, and health spending accounts
- take the administrative work away
- significantly contain costs, simplify administration and enhance convenience
- we’re re-thinking the relationship between insurers and their customers and the ways in which they interact
1.11.2 Comparison and shopping guides
- we help you to find the best deal
- receive a tailored quote
- algorithm seeks lowest premiums across major insurers and shows customized results
- an integrated comparison shopping portal for health
- identify insurance companies with the coverage, service level, and pricing to suit their unique needs
- compare products quickly and simply
- easy-to-use search
- easy and sensible comparisons
- instant, customized rate quotes
- fast, accurate and actionable and customized rate quotes
- find the right products at the best prices, helping save time and money
- see quotes you can trust, because we work directly with the insurance companies to get them for you
1.11.3 Online and mobile insurance and insurance markets places
- online insurer, end to end, from selling to claims
- online supermarket for insurance solutions
- online insurance policy aggregator that offers consumers life and non-life insurance policies across several categories
- the first direct-to-consumer online marketplace
- first online independent renters insurance platform
- leader in the digital distribution of travel insurance
- first online car insurance shopping platform, which instantly verifies customer data to provide intuitive and integrated user experience
- automated insurance agent dedicated to making insurance quicker, easier and more personal than ever before
- transform the insurance experience for small businesses, giving them a process that’s online, transparent, fast and complete
- mobile-delivered insurance in the developing world
- mobile-first solution to quickly and easily get a price quote for insurance coverage
- mobile insurance claims solution
- redefining how insurance is priced and delivered
- a more connected healthcare experience
- simple, no-hassle health insurance marketplace and administrative platform for small businesses
- track insurance and report & track claims on-line
- a web-based platform that enables its users to pool their car insurance premiums online to save money
- a genuine alternative to insurance for crisis events
- cut straight to insurance that will actually cover your unique situation
- a free, members-only service that helps you find insurance for the things in your life that you care about or are out of the ordinary
- we want to give our customers an easy to use, customer centric way to get insurance
- we provide the tools and services to anyone to create their own custom Insurance policies
- we have built technology to simplify the shopping and organization of your insurance
1.11.4 Peer-to-peer insurance
- online peer-to-peer insurance…lowering annual insurance premiums by up to 50%
- first insurance company designed around peer-to-peer technology
- pools friends & trusted acquaintances or adds users to existing groups of 5 or more for car insurance
- […] has nothing to gain by denying your claims. In fact, we simply can’t do that. It’s you and your teammates who have exclusive control.
- you and your teammates cover each other. If you submit a claim within your team, your teammates pay it
- your team doesn’t have the expenses of a regular insurance company. Oh, and you keep 100% of your money if there are no claims in your team.
- there are no pools in […]. You get coverage directly from your teammates
1.11.5 Technology solutions for insurers
- help insurers deepen their engagement with consumers
- help insurers replace their legacy core systems and increase their operational efficiencies and speed to market
- built with technology at its core
- easy, low cost way to launch, distribute and manage insurance products anywhere in the world
- solution to a global insurance industry seeking to modernize its systems
1.11.6 Claims handling and adjusting
- simplifies and accelerates claims management through the broadest range of technology solutions
- medical bill review software delivered in with leading cloud based technology
- our products and services enable better decisions and achieve better outcomes
- expert medical bill review services, using the most advanced technology
1.11.7 New coverages and risk products
- a better way to insure your phone
- provides insurance for smart phones, laptops, cameras and tablets
- standalone car rental insurance
- allows drivers to get insured on a friend’s car for as little as an hour from a mobile device
- on-demand, micro-duration insurance coverage for single items and possessions
- on-demand insurance for the on-demand economy, offering insurance that turns on and off when needed
- micro-duration life insurance coverage during airplane travel
- providing a self-insurance platform so smaller companies can enjoy the benefits of self-insurance
- power & economy of bulk purchases delivered to online communities
- software app for home remodeling that provides an insurance product to guarantee the outcome of projects
- an on-demand insurance platform. It works like Uber and Airbnb.
- protect just the things you want - exactly when you want - entirely from your phone
1.11.8 Safety, risk management, UBI, auto safety
- integrating technology into all aspects of healthcare insurance, including continuous, real-time monitoring to prevent hospital admissions
- harnesses the power of behavioral economics and the essence of the sharing economy
- comparison shopping platform for usage-based insurance
- the forefront of the insurance telematics wave
- the world’s most accurate mobile app to track driver behavior and replace traditional black box
- monitor commercial drivers’ alertness
- road safety applications that offer driver feedback
- empower drivers to make better driving-related decisions
- location tracking, driver scoring, alert and location sharing services
- unlock and make use of the world’s driving data
- access, analyze, and manage driving data at a massive scale
- changes the way people experience driving
- turns your daily commute into a dynamic social activity
- shaping the future of driving safety - through data and technology
1.11.10 Other innovations
- streamlined communication between insurance brokers and carriers
- real-time 3d and 2d maps for property assessment
- mathematical modeling and algorithms to detect fraudulent behavior
- predictive models of legal risk
- offer investors bespoke exposure to insurance risk